As a new CVT / RVT one of the things that really surprised me was the number of treatable trauma or acute disease cases that I've seen end in euthanasia due to the owners not having the money for treatment. While it is easy to get angry at the owner I think it's a bit more complicated than that. Most of the time we have no idea what our clients' histories are. Who knows if they lost their job 6 months ago, got divorced, or maybe even lost a spouse which left them in the situation of having a pet without enough money for advanced treatments. I mean, on our salaries, many of us should be able to relate, right? And those with parents, friends, or relatives willing to loan or give money in emergencies should count themselves lucky. Without them or our spouses who's income we depend on, I think all of us could easily find ourselves in their shoes.
So, what to do about it? Our clinic offers CARE credit, but many clients are declined. We also have a donor who's willing to pay for select animals and we do our best to work with any others as far as discounts, or payment plans are concerned. For the rest, the only answer is often euthanasia and after seeing several in the span of 3 weeks I decided to do some digging. I wondered if there was a charity out there to help pay for veterinary medical bills or how difficult it might be to create one. Turns out there is at least one out there called Red Rover.
I don't know much about them yet and can't fathom how I'd find the time to create a charity of my own, but I'm still researching and mulling options in my head. Ideally we'd save them all, but with my background in shelter medicine I completely understand that this is not possible. Still, it's important to try.
Information for Vet Techs and Vet Assistants as well as cool cases to share and discuss.
Saturday, December 8, 2012
Saturday, October 6, 2012
If and when to neuter your dog
This article is aimed at male dogs only. Female dogs should be spayed before their first heat due to the dramatic reduction in their risk for mammary tumors. Aside from the fact that mammary tumors are common and up to 50% of them are malignant, I can tell you that I've seen many mammary tumor surgeries and it is heartbreaking to see an animal undergo and recover from surgery to remove an entire chain of mammary glands. They are cut from their chest to their groin which results in a painful recovery and a lot of management to control swelling. It's not fun for the animal or the owner.
Males are a little different. The benefits of neutering a male are:
PS:
I know seeing cancers in the "risks" column is quite scary, but keep in mind that these are small increases of already small risks. And keep in mind that people tend to write to catch your attention online. A headline of "Neutering doubles the risk of cancer" would strike fear in the heart of any pet owner, but can be quite misleading if the risk goes from 0.01% to 0.02%. Sure, the risk doubled, but it's still incredibly low.
Males are a little different. The benefits of neutering a male are:
- eliminates the risk of testicular cancer
- decreased risk of prostate disorders (up to 80% of unneutered males develop some sort of prostatic disease or cancer although it is usually not malignant)
- decreased risk of perianal fistulas (lesions and abscesses that occur around the anus which tend to recur and become chronic, if surgery is necessary there is a risk of fecal incontinence)
- decreased risk of hernias
- fewer behavioral problems (decreased aggression, roaming, and shorter attention span)
- anesthesia (very low risk for healthy dogs, even lower with proper pre-surgical bloodwork)
- early neutering MAY increase the risk of osteosarcoma (malignant bone cancer) in giant breed dogs
- increased risk of hemangiosarcoma (cancer of the blood vessels, that's an increase of 3% chance to 4.5% chance AT MOST)
- increased risk of osteosarcoma (the earlier the castration the higher the risk; the average lifetime risk of Great Danes is 4%)
PS:
I know seeing cancers in the "risks" column is quite scary, but keep in mind that these are small increases of already small risks. And keep in mind that people tend to write to catch your attention online. A headline of "Neutering doubles the risk of cancer" would strike fear in the heart of any pet owner, but can be quite misleading if the risk goes from 0.01% to 0.02%. Sure, the risk doubled, but it's still incredibly low.
Friday, October 5, 2012
An owner's guide to "bloat" or "GDV".
If you own a Great Dane, German Shepherd, English bulldog, Weimaraner, Rottweiler, or other deep chested breed you should probably be familiar with the signs of bloat.
Signs:
- Restlessness (pacing, trying to sit or lay down and then getting back up, generally acting uncomfortable)
- Drooling
- Retching (attempting to vomit, but nothing comes out)
- Looking bloated (the abdomen or stomach looks larger than normal
What to do:
The above signs are very general and could mean a number of other things besides bloat, but because bloat can kill a dog very quickly it's important to not take the signs lightly.- Check gum color: Bloat causes shock and a sign of shock is pale or dark red mucous membranes. The easiest way to check for this is to take a look at your dog's gums. They should be nice and pink like your own gums. Some dogs naturally have brown or black gums, in this case you can take a look at their tongue and/or the inside of their lower eyelid. The key is to pick a place to look and make sure you know what normal looks like so that if something happens you can recognize the change.
- If you have the slightest concern that your dog is bloating you need to take it to the nearest vet immediately. Bloat is a life-threatening condition. The sooner you can get the dog in the more likely it will survive.
Prevention:
The cause of bloat is unknown, so much of the advice about prevention is unproven:- Feeding more than once a day: its better to feed two or three smaller meals rather than one large meal a day.
- Do not allow gulping of food or water.
- Put food and water bowls on the floor rather than using raised bowls.
- Limit exercise for an hour before and after feeding.
- Don't encourage the dog to roll over. Dogs roll over on their own all the time, and it is low-risk, but it's best not make that part of any games or teach them to do so as a trick.
- If you own a Great Dane talk to your vet about stomach tacking. It's not a guarantee against bloat, but it does improve your dog's chances of surviving if bloat does occur.
Planning ahead:
In my opinion, any Great Dane owner should have a plan in place for dealing with bloat. Studies show that 25% - 40% of Great Danes will bloat in their lifetime. Being prepared will help you stay calm and improve your dog's chances of survival.- The #1 thing to do is: know where your nearest emergency vet is and how to get there. If your vet isn't open 24 hours/365 days a year you should find the nearest vet who is and have the address and directions pre-printed.
- If the nearest emergency vet is more than 20 minutes away or so you may want to talk to your vet about measures you can take yourself to relieve the pressure in the stomach while transporting the dog for further treatment. This often involves having a soft rubber or plastic tube that can be put down the dog's throat and into the stomach to release the gas. Extreme caution must be used when doing this, however, because when bloat advances the stomach often twists which closes it off so the tube cannot pass. Attempting to push the tube into the stomach with any force can tear the esophagus and kill the dog. Again, if this is something you feel you might have to do, please speak with your vet to find out how to do this properly or to discuss the risks vs benefits of doing this at all.
Monday, September 3, 2012
Reading a Chemistry, Cl / Chlorine
Chloride is an extracellular anion that helps with water balance (osmality), is necessary for spinal fluid production, and helps transport other ions across cellular membranes. Chloride is a required nutrient and is often balanced with sodium.
Since Cl and Na both control osmality they'll shift out of the blood stream when water moves out. For this reason, Chloride changes are often corrected by using the following formula: Corrected Cl = (normal Na/measured Na) x measured C.
Increased chlorine or "hyperchloremia" may be caused by:
- Shift of water:If the corrected Chloride falls in the normal range the change is due to a shift of water within the body.
-Pseudohyperchloremia: due to the administration of or a dietary increase of bromide which is read as chloride by some Chem machines.
-Drugs: diuretics will cause hyperchloremia as will the administration of chloride-containing fluids.
-Kidney issues: renal failure or renal tubular acidosis.
-Addison's disease
-Diabetic ketoacidosis
-Chronic respiratory alkalosis
Decreased chlorine or "hypochloremia" may be caused by:
-Vomiting: if chloride is low relative to sodium vomiting may be the reason. Part of what makes stomach acid so acidic is an increase of chloride, so if chloride is being lost without sodium, vomiting could be the cause.
-Intestinal issues: such as diarrhea. Chloride is absorbed in the large intestine of horses, so if there's an absorption issue chloride may be low.
-Kidney disease: may cause hypochloremia, especially in cattle.
-Too much sodium: such as from the administration of sodium-containing fluids may cause chloride to be low compared to sodium.
Since Cl and Na both control osmality they'll shift out of the blood stream when water moves out. For this reason, Chloride changes are often corrected by using the following formula: Corrected Cl = (normal Na/measured Na) x measured C.
Increased chlorine or "hyperchloremia" may be caused by:
- Shift of water:If the corrected Chloride falls in the normal range the change is due to a shift of water within the body.
-Pseudohyperchloremia: due to the administration of or a dietary increase of bromide which is read as chloride by some Chem machines.
-Drugs: diuretics will cause hyperchloremia as will the administration of chloride-containing fluids.
-Kidney issues: renal failure or renal tubular acidosis.
-Addison's disease
-Diabetic ketoacidosis
-Chronic respiratory alkalosis
Decreased chlorine or "hypochloremia" may be caused by:
-Vomiting: if chloride is low relative to sodium vomiting may be the reason. Part of what makes stomach acid so acidic is an increase of chloride, so if chloride is being lost without sodium, vomiting could be the cause.
-Intestinal issues: such as diarrhea. Chloride is absorbed in the large intestine of horses, so if there's an absorption issue chloride may be low.
-Kidney disease: may cause hypochloremia, especially in cattle.
-Too much sodium: such as from the administration of sodium-containing fluids may cause chloride to be low compared to sodium.
Sunday, September 2, 2012
Reading a Chemistry, K / Potassium
Potassium is an intracellular cation although it is passed across cell membranes to alter cell polarity. It plays a key role in cardiac rhythm and rate, the kidney's ability to handle sodium, and acid-base metabolism. Potassium and sodium absorption and excretion are usually tied to one another, so excesses or deficiencies of one of these electrolytes often effects the other.
Increased potassium or "hyperkalemia" may occur due to:
-Artifact: due to sample clotting (K is released for platelets as they clot) or hemolysis especially in horses and pigs (since potassium is found in high concentrations inside of cells, when the cells are lysed the potassium leaks out making it appear that there is more potassium in the extracellular fluid than expected)
-Cell rupture: due to over-exercise, tissue necrosis, etc.
-Leukocytosis: very high WBC counts can result in hyperkalemia due to cell leakage.
-Drugs: Trimethoprim induces hyperkalemia by inhibiting sodium resorption in the cortical collecting ducts of the kidney.
-Metabolic acidosis: potassium gets redistributed as the body tries to deal with the acidosis.
-Decreased renal excretion: in cases of oliguria or anuria such as blocked toms.
-Ruptured urinary bladder: if this is the case Na and Cl will be low (hyponatremia and hypochloremia)
-Inherited conditions: such as Hyperkalemic polymyopathy of horses.
*Observe your patient: Hyperkalemia will result in cardiac malfunction and generalized muscle weakness.
Decreased potassium or "hypokalemia" may occur due to:
-Artifact: lipemia may cause a pseudohypokalemia
-Decreased intake: due to dietary insufficiency, anorexia,
-Redistribution: this may occur due to hormones including insulin and catecholamine so it can be brought on via bolus glucose administration, stress, or excitement.
-Fecal loss: if large amounts of sodium are being absorbed in the large intestine large amounts of potassium may be lost.
-Renal losses: Increased GFR in the kidney: this will decrease reabsorption leading to hypokalemia. Increased sodium excretion by the kidney: potassium is excreted along with sodium.
-Metabolic alkalosis
-Mineralcorticoids: such as aldosterone increase renal tubular resorption of sodium can result in potassium excretion by the kidney. This can be due to administration of drugs, neoplasia, or other disorders.
*Observe your patient: Hypokalemia can result in restlessness, generalized muscle weakness, cardiac arrhythmia and death.
Increased potassium or "hyperkalemia" may occur due to:
-Artifact: due to sample clotting (K is released for platelets as they clot) or hemolysis especially in horses and pigs (since potassium is found in high concentrations inside of cells, when the cells are lysed the potassium leaks out making it appear that there is more potassium in the extracellular fluid than expected)
-Cell rupture: due to over-exercise, tissue necrosis, etc.
-Leukocytosis: very high WBC counts can result in hyperkalemia due to cell leakage.
-Drugs: Trimethoprim induces hyperkalemia by inhibiting sodium resorption in the cortical collecting ducts of the kidney.
-Metabolic acidosis: potassium gets redistributed as the body tries to deal with the acidosis.
-Decreased renal excretion: in cases of oliguria or anuria such as blocked toms.
-Ruptured urinary bladder: if this is the case Na and Cl will be low (hyponatremia and hypochloremia)
-Inherited conditions: such as Hyperkalemic polymyopathy of horses.
*Observe your patient: Hyperkalemia will result in cardiac malfunction and generalized muscle weakness.
Decreased potassium or "hypokalemia" may occur due to:
-Artifact: lipemia may cause a pseudohypokalemia
-Decreased intake: due to dietary insufficiency, anorexia,
-Redistribution: this may occur due to hormones including insulin and catecholamine so it can be brought on via bolus glucose administration, stress, or excitement.
-Fecal loss: if large amounts of sodium are being absorbed in the large intestine large amounts of potassium may be lost.
-Renal losses: Increased GFR in the kidney: this will decrease reabsorption leading to hypokalemia. Increased sodium excretion by the kidney: potassium is excreted along with sodium.
-Metabolic alkalosis
-Mineralcorticoids: such as aldosterone increase renal tubular resorption of sodium can result in potassium excretion by the kidney. This can be due to administration of drugs, neoplasia, or other disorders.
*Observe your patient: Hypokalemia can result in restlessness, generalized muscle weakness, cardiac arrhythmia and death.
Reading a Chemistry, Na / Sodium
Sodium is an extracellular cation. It drives the movement of fluid between epithelial surfaces within the body and also plays a key role in creating neural impulses, muscle contractions, and secretions.
Increased sodium "hypernatremia" may be caused by:
-Excessive intake: dietary or via fluid therapy. Signs of this often include increased urine volume and signs of dehydration.
-Dehydration: (relative increase meaning that the concentration is high only because of the water loss and referred to as pseudohypernatremia). In many cases of dehydration, however, sodium levels are normal.
Decreased sodium "hyponatremia" may be caused by:
-Artifact: if the sample was lipemic or hyperproteinemic
-Excessive water intake: In this case the GFR is increased so that sodium cannot be resorbed.
-Water retention: due to congestive heart failure, liver disease, nephrotic syndrome or advanced renal failure.
-Renal issues: lack of aldosterone, proximal renal tubule dysfunction (resulting in reduced sodium absorption) in renal disease (especially in horses and cattle), osmotic losses due to polyuria (diabetes mellitus), and diuretic therapy. Cattle with renal failure have a consistent moderate to marked hyponatremia.
-Gastrointestinal issues: sodium may be lost due to diarrhea, especially in cattle.
-Addison's disease (hypoadrenocorticism):
Increased sodium "hypernatremia" may be caused by:
-Excessive intake: dietary or via fluid therapy. Signs of this often include increased urine volume and signs of dehydration.
-Dehydration: (relative increase meaning that the concentration is high only because of the water loss and referred to as pseudohypernatremia). In many cases of dehydration, however, sodium levels are normal.
Decreased sodium "hyponatremia" may be caused by:
-Artifact: if the sample was lipemic or hyperproteinemic
-Excessive water intake: In this case the GFR is increased so that sodium cannot be resorbed.
-Water retention: due to congestive heart failure, liver disease, nephrotic syndrome or advanced renal failure.
-Renal issues: lack of aldosterone, proximal renal tubule dysfunction (resulting in reduced sodium absorption) in renal disease (especially in horses and cattle), osmotic losses due to polyuria (diabetes mellitus), and diuretic therapy. Cattle with renal failure have a consistent moderate to marked hyponatremia.
-Gastrointestinal issues: sodium may be lost due to diarrhea, especially in cattle.
-Addison's disease (hypoadrenocorticism):
Reading a Chemistry, ALP
ALP can help diagnose cholestasis, but it is not liver specific in most animals. It is also found in bone, intestine, kidney, mammary and placental tissues. So when ALP is elevated the origin could be in the liver or any of these other tissues.
ALP elevation may be caused by:
-Cholestasis
-Liver disease
-Bone disease: increased osteoblastic activity due to hyperparathyroidism, osteosarcoma, a healing fracture (in dogs).
-Increased cortisol: due to steroid administration (such as prednisone) or due to Cushings (hyperadrenocorticism). This is less likely in cats
ALP elevation may be caused by:
-Cholestasis
-Liver disease
-Bone disease: increased osteoblastic activity due to hyperparathyroidism, osteosarcoma, a healing fracture (in dogs).
-Increased cortisol: due to steroid administration (such as prednisone) or due to Cushings (hyperadrenocorticism). This is less likely in cats
Reading a Chemistry, ALT
ALT is an enzyme that is found on the inside of liver cells. So, when liver cells get damaged it leaks out and the levels become elevated in the blood. ALT is specific to the liver, so it is a good indicator of liver damage, but it is only useful in dogs, cats, rabbits and primates. Large animals have very little ALT so SDH and GLDH are used instead.
Increased ALT can be caused by:
-Artifact: In cats hemolysis can result in elevated ALT levels when no liver damage is present.
-Drugs: Anti-seizure medication such as primidone, phenobarbitone, dilantin will increase ALT levels up to four times normal. Corticosteroids increase ALT up to 2-3 x normal. Any other drugs that cause hepatotoxicity may also raise ALT such as: tetracycline in cats, caparsolate in dogs, or acetaminophen.
-Liver disease: conditions that alter cell membrane permeability or cause necrosis will cause ALT levels to rise and ALT will usually be higher than AST in cases of liver disease.
-Bile duct obstruction: if bile backs up it will begin breaking down tissue which may lead to elevated ALT.
-Trauma: if liver cells are hurt or destroyed ALT levels may become elevated.
-Muscle disease: in severe cases such as ischemic myopathy in cats, muscular dystrophy in dogs ALT my become elevated but AST and CK levels will rise to a much greater degree.
-Cancer: hepatic neoplasia can also cause ALT levels to rise although in this case AST is usually higher than ALT.
Decreased ALT can be caused by:
There is no such thing as ALT levels that are "too low".
Increased ALT can be caused by:
-Artifact: In cats hemolysis can result in elevated ALT levels when no liver damage is present.
-Drugs: Anti-seizure medication such as primidone, phenobarbitone, dilantin will increase ALT levels up to four times normal. Corticosteroids increase ALT up to 2-3 x normal. Any other drugs that cause hepatotoxicity may also raise ALT such as: tetracycline in cats, caparsolate in dogs, or acetaminophen.
-Liver disease: conditions that alter cell membrane permeability or cause necrosis will cause ALT levels to rise and ALT will usually be higher than AST in cases of liver disease.
-Bile duct obstruction: if bile backs up it will begin breaking down tissue which may lead to elevated ALT.
-Trauma: if liver cells are hurt or destroyed ALT levels may become elevated.
-Muscle disease: in severe cases such as ischemic myopathy in cats, muscular dystrophy in dogs ALT my become elevated but AST and CK levels will rise to a much greater degree.
-Cancer: hepatic neoplasia can also cause ALT levels to rise although in this case AST is usually higher than ALT.
Decreased ALT can be caused by:
There is no such thing as ALT levels that are "too low".
Saturday, September 1, 2012
Reading a Chemistry, Chol / Cholesterol
Cholesterol is form of lipid that is made by the liver. It is a component of cell membranes and is used to create hormones as well.
Causes of high cholesterol include:
-Hormone disorders: hypothyroidism or hyperadrenocorticism may cause high cholesterol with normal serum triglycerides.
-Kidney disease: such as nephrotic syndrome
-Pancreatitis: in this case both serum triglycerides and cholesterol will be high.
-Diabetes mellitus: in this case both serum triglycerides and cholesterol will be high. Of course, blood glucose should be checked to further confirm this as a possible diagnosis.
-Liver issues: especially cholestasis. This is because the liver is primarily responsible for cholesterol excretion. With liver issues both serum triglycerides and cholesterol will be high.
* It is worth noting that high cholesterol does not put animals at risk for heart or blood vessel problems like it does in humans.
Causes of low cholesterol include:
-Liver issues: the liver synthesizes cholesterol, so if it isn't functioning properly blood cholesterol may be low. If cholestasis is present as well, however, cholesterol cannot be excreted so the lack of synthesis and lack of excretion may cancel each other out and give a normal result.
-Hyperthyroidism
-Malabsorption: such as EPI (exocrine pancreatic insufficiency). In this case serum triglycerides will also be low.
Causes of high cholesterol include:
-Hormone disorders: hypothyroidism or hyperadrenocorticism may cause high cholesterol with normal serum triglycerides.
-Kidney disease: such as nephrotic syndrome
-Pancreatitis: in this case both serum triglycerides and cholesterol will be high.
-Diabetes mellitus: in this case both serum triglycerides and cholesterol will be high. Of course, blood glucose should be checked to further confirm this as a possible diagnosis.
-Liver issues: especially cholestasis. This is because the liver is primarily responsible for cholesterol excretion. With liver issues both serum triglycerides and cholesterol will be high.
* It is worth noting that high cholesterol does not put animals at risk for heart or blood vessel problems like it does in humans.
Causes of low cholesterol include:
-Liver issues: the liver synthesizes cholesterol, so if it isn't functioning properly blood cholesterol may be low. If cholestasis is present as well, however, cholesterol cannot be excreted so the lack of synthesis and lack of excretion may cancel each other out and give a normal result.
-Hyperthyroidism
-Malabsorption: such as EPI (exocrine pancreatic insufficiency). In this case serum triglycerides will also be low.
Reading a Chemistry, Glob / Globulins
Globulins are the second most common protein in serum or plasma. They are responsible for the body's immune functions.
Increased globulins or "hyperglobulinemia" may result from:
-Immune system stimulation: from infection or allergies.
-Stress
-Dehydration: this is a relative increase meaning that the amount of globulin is normal, but it is more concentrated due to the lack of water. This is likely the case if albumin is also increased.
-Liver disease
-Heart disease
-Arthritis
-Diabetes
Decreased globulins may result from:
-Immune system suppression: due to corticosteroid use,r stress, or infectious disease.
Increased globulins or "hyperglobulinemia" may result from:
-Immune system stimulation: from infection or allergies.
-Stress
-Dehydration: this is a relative increase meaning that the amount of globulin is normal, but it is more concentrated due to the lack of water. This is likely the case if albumin is also increased.
-Liver disease
-Heart disease
-Arthritis
-Diabetes
Decreased globulins may result from:
-Immune system suppression: due to corticosteroid use,r stress, or infectious disease.
Reading a Chemistry, Albumin
Albumin is made by the liver and is the most plentiful of the plasma or serum proteins. As a natural colloid it plays a major role in maintaining vascular volume.
Causes of increased albumin:
-Dehydration: is the only cause of increased albumin.
Causes of decreased albumin:
-Liver issues: if liver function is impaired albumin may not be produced.
-Kidney disease: albumin may be lost by a leaky glomerulus
-Blood loss: even if RBC's are normal. The spleen sequesters a reserve of red blood cells, but there is no such reserve for albumin, so shortly after a major blood loss albumin will be decreased, but the red blood cell count may not be.
Causes of increased albumin:
-Dehydration: is the only cause of increased albumin.
Causes of decreased albumin:
-Liver issues: if liver function is impaired albumin may not be produced.
-Kidney disease: albumin may be lost by a leaky glomerulus
-Blood loss: even if RBC's are normal. The spleen sequesters a reserve of red blood cells, but there is no such reserve for albumin, so shortly after a major blood loss albumin will be decreased, but the red blood cell count may not be.
Reading a Chemistry, Phosphorous
Phosphorous exists in the intracellular fluid, in bone, and elsewhere. It is usually balanced with calcium in the body so it's regulated by PTH (parathyroid hormone) and calcitonin. It also plays a part in acid-base metabolism.
Increased phosphorous "hyperphosphatemia" may be caused by:
-Cellular damage: due to the intracellular phosphorous leaking out.
-Over-administration of phosphorous: via phosphorous containing fluids, foods, or enemas.
-Renal issues: reductions in renal blood flow or GFR will cause more phosphorous than normal to be reabsorbed.
-Ruptured bladder: phosphorous from the urine is reabsorbed from the abdomen and ends up back in the blood.
Decreased phosphorous "hypophosphatemia" may be caused by:
-Increased use: increased cellular uptake of phosphorous due to accelerated metabolism
-Decreased intake
-Over-administration of binders: such as during treatment for chronic renal failure or antacids that bind with phosphate.
-Alkalosis
Increased phosphorous "hyperphosphatemia" may be caused by:
-Cellular damage: due to the intracellular phosphorous leaking out.
-Over-administration of phosphorous: via phosphorous containing fluids, foods, or enemas.
-Renal issues: reductions in renal blood flow or GFR will cause more phosphorous than normal to be reabsorbed.
-Ruptured bladder: phosphorous from the urine is reabsorbed from the abdomen and ends up back in the blood.
Decreased phosphorous "hypophosphatemia" may be caused by:
-Increased use: increased cellular uptake of phosphorous due to accelerated metabolism
-Decreased intake
-Over-administration of binders: such as during treatment for chronic renal failure or antacids that bind with phosphate.
-Alkalosis
Reading a Chemistry, Ca / Calcium
Calcium is balanced in the body by ParaThyroid Hormone (PTH) which stimulates bone breakdown in order to increase the calcium levels in the blood when they are low and calcitonin which stimulates the storage of calcium in the bone thereby decreasing blood calcium.
Increased blood calcium "hypercalcemia" may be caused by:
-Overactive parathyroid: (hyperparathyroidism) due to cancer or hypoadrenocorticism.
-Cancer: Increased calcium raises a red flag for lymphoma, myeloma, osteosarcoma, some adenocarcinomas, or other types of cancers.
-Diet: vitamin D toxicity.
-Renal failure
Decreased blood calcium "hypocalcemia" may be caused by:
-Eclampsia: the demands of milk production may result in hypocalcemia.
-Diet: calcium or vitamin D deficiency.
-Loop diuretics: result in loss of calcium.
-Stress
-Pancreatitis
-Renal failure
-Tissue degradation: as happens with circulatory shock or heat stress.
-Hypercalcitoninism: too much calcitonin (rare).
-Secondary to other issues: such as hypoalbuminemia or acid-base imbalances
Increased blood calcium "hypercalcemia" may be caused by:
-Overactive parathyroid: (hyperparathyroidism) due to cancer or hypoadrenocorticism.
-Cancer: Increased calcium raises a red flag for lymphoma, myeloma, osteosarcoma, some adenocarcinomas, or other types of cancers.
-Diet: vitamin D toxicity.
-Renal failure
Decreased blood calcium "hypocalcemia" may be caused by:
-Eclampsia: the demands of milk production may result in hypocalcemia.
-Diet: calcium or vitamin D deficiency.
-Loop diuretics: result in loss of calcium.
-Stress
-Pancreatitis
-Renal failure
-Tissue degradation: as happens with circulatory shock or heat stress.
-Hypercalcitoninism: too much calcitonin (rare).
-Secondary to other issues: such as hypoalbuminemia or acid-base imbalances
Reading a Chemistry, Crea / Creatinine
Creatinine is a product of muscle breakdown. In healthy animals the rate of muscle breakdown and, therefore, creatinine release into the blood is fairly steady. It is filtered out of the blood by the kidney and reabsorption does not occur as it does with BUN. Because it is not influenced by an animal's diet or the GFR of the kidney, it is a more reliable test for kidney function than BUN although they are often both analyzed together.
Increased creatinine may be caused by:
-Kidney failure: if the kidney isn't functioning properly it won't filter the creatinine out of the blood and it will build up.
-Muscle damage: increased creatinine values would be expected in animals with muscle damage such as hit-by-car cases or animals that have recently been over-exercised.
Decreased creatinine levels may be caused by:
-Decreased muscle mass: less muscle will result in less metabolism and, therefore, less creatinine produced.
Increased creatinine may be caused by:
-Kidney failure: if the kidney isn't functioning properly it won't filter the creatinine out of the blood and it will build up.
-Muscle damage: increased creatinine values would be expected in animals with muscle damage such as hit-by-car cases or animals that have recently been over-exercised.
Decreased creatinine levels may be caused by:
-Decreased muscle mass: less muscle will result in less metabolism and, therefore, less creatinine produced.
Reading a Chemistry, BUN / Blood Urea Nitrogen
When the body digests protein ammonia is produced as a waste product. If you can imagine the ammonia you buy at the store, it is a very caustic substance that definitely should not be coursing around the body. So, the liver quickly absorbs it and converts it to urea, a less toxic waste product. The urea is released into the blood and then filtered out by the kidney and concentrated to make urine. BUN, then, is often used to check kidney function.
Increased BUN may be caused by:
-Kidney disease: BUN will build up in the blood if the kidneys are not filtering it out properly.
-Decreased GFR: or glomerular filtration rate. This means the kidney is filtering the blood more slowly than usual. This allows substances such as BUN to be re-absorbed at a greater rate than they would normally be, resulting in higher than usual concentrations of BUN in the blood.
-High protein diets: more protein equals more waste. Because this test can be influenced by an animal's diet it isn't reliable on its own. This is why BUN and Creatinine are often looked at together.
-Tissue damage: when the body's own proteins are damaged or destroyed by fever or necrosis it digests them. Large amounts of damage may increase the BUN.
Decreased BUN may be caused by:
-Low protein diet: less protein means less BUN produced. Because this test can be influenced by an animal's diet it isn't reliable on its own. This is why BUN and Creatinine are often looked at together.
-Liver disease: if the liver is not functioning it won't produce the urea that results in BUN. Of course, if this is suspected ammonia should be looked at as well. If it isn't being converted to BUN, than it should be building up in the blood.
Increased BUN may be caused by:
-Kidney disease: BUN will build up in the blood if the kidneys are not filtering it out properly.
-Decreased GFR: or glomerular filtration rate. This means the kidney is filtering the blood more slowly than usual. This allows substances such as BUN to be re-absorbed at a greater rate than they would normally be, resulting in higher than usual concentrations of BUN in the blood.
-High protein diets: more protein equals more waste. Because this test can be influenced by an animal's diet it isn't reliable on its own. This is why BUN and Creatinine are often looked at together.
-Tissue damage: when the body's own proteins are damaged or destroyed by fever or necrosis it digests them. Large amounts of damage may increase the BUN.
Decreased BUN may be caused by:
-Low protein diet: less protein means less BUN produced. Because this test can be influenced by an animal's diet it isn't reliable on its own. This is why BUN and Creatinine are often looked at together.
-Liver disease: if the liver is not functioning it won't produce the urea that results in BUN. Of course, if this is suspected ammonia should be looked at as well. If it isn't being converted to BUN, than it should be building up in the blood.
Reading a Chemistry, Glucose
Glucose is commonly called blood sugar. It can be tested with a Chem machine or with a handheld glucometer. It should be noted, however, that due to various reasons, glucometer readings may vary greating from those found on a Chem test. For monitoring purposes, a tech should choose one machine and use it exclusively to get consistent results; ideally the Chem machine may be used for accuracy or the owner's glucometer may be used for consistency.
Increased glucose or "hyperglycemia" may be caused by:
-Diabetes mellitus: Glucose is often used to indirectly monitor insulin. This is because cells cannot consume the glucose in the blood without the presence of insulin, often described as the "key" to allow glucose into the cell. So, when the body stops producing insulin (diabetes melletus), glucose cannot be used by the cells and begins building up in the blood. Hyperglycemia on a fasting blood test very likely indicates diabetes mellitus.
-Pancreatitis
-Drug-induced: prolonged use of steroids or morphine may cause hyperglycemia.
-Stress: this means that more than one blood test may be needed to diagnose diabetes mellitus.
Decreased glucose or "hypoglycemia" may be caused by:
-Too much insulin given: if the animal is being treated for diabetes the cause of low blood sugar is likely that the animal was given too much insulin relative to what it ate. The short-term fix might be giving an extra meal in minor cases, giving sugar water, or in the case of dangerously low blood sugar IV administration of dextrose or in a home setting, rubbing karo syrup (corn syrup) on the gums and mucous membranes of the mouth.
-Starvation: the body runs out of fuel and cannot keep up with the demand for glucose.
-Artifact: when blood is drawn it contains living cells. If those cells are left to sit, even after spinning, before the test is run, they continue to use glucose. So, if you want a good glucose reading the blood must be processed and the test run promptly or, if a delay is unavoidable, you can spin the blood, then draw off the serum and freeze it for later testing.
-Advanced liver disease: the liver produces and stores glycogen which can be quickly converted to glucose, and thus serves as a reserve for glucose. If over 70% of the liver's function is lost it may not be able to produce or store this reserve and hypoglycemia may result.
-Insulinoma: an insulin-producing tumor that results in increased glucose use within the body.
-Sepsis: infection can cause increased glucose utilization.
-Pregnancy toxemia: especially in bovine, in late pregnancy, ketosis may occur due to the demands of the growing fetus.
-Addison's disease: results in decreased glucogenesis and increased glucose use by skeletal muscle.
Increased glucose or "hyperglycemia" may be caused by:
-Diabetes mellitus: Glucose is often used to indirectly monitor insulin. This is because cells cannot consume the glucose in the blood without the presence of insulin, often described as the "key" to allow glucose into the cell. So, when the body stops producing insulin (diabetes melletus), glucose cannot be used by the cells and begins building up in the blood. Hyperglycemia on a fasting blood test very likely indicates diabetes mellitus.
-Pancreatitis
-Drug-induced: prolonged use of steroids or morphine may cause hyperglycemia.
-Stress: this means that more than one blood test may be needed to diagnose diabetes mellitus.
Decreased glucose or "hypoglycemia" may be caused by:
-Too much insulin given: if the animal is being treated for diabetes the cause of low blood sugar is likely that the animal was given too much insulin relative to what it ate. The short-term fix might be giving an extra meal in minor cases, giving sugar water, or in the case of dangerously low blood sugar IV administration of dextrose or in a home setting, rubbing karo syrup (corn syrup) on the gums and mucous membranes of the mouth.
-Starvation: the body runs out of fuel and cannot keep up with the demand for glucose.
-Artifact: when blood is drawn it contains living cells. If those cells are left to sit, even after spinning, before the test is run, they continue to use glucose. So, if you want a good glucose reading the blood must be processed and the test run promptly or, if a delay is unavoidable, you can spin the blood, then draw off the serum and freeze it for later testing.
-Advanced liver disease: the liver produces and stores glycogen which can be quickly converted to glucose, and thus serves as a reserve for glucose. If over 70% of the liver's function is lost it may not be able to produce or store this reserve and hypoglycemia may result.
-Insulinoma: an insulin-producing tumor that results in increased glucose use within the body.
-Sepsis: infection can cause increased glucose utilization.
-Pregnancy toxemia: especially in bovine, in late pregnancy, ketosis may occur due to the demands of the growing fetus.
-Addison's disease: results in decreased glucogenesis and increased glucose use by skeletal muscle.
Reading a CBC: TP / Total Protein or TS / Total Solids
Total protein refers to the total serum or plasma protein and can be determined by machine or very simply by taking the microhematocrit tube that you used for your PCV and breaking it at the level of the serum or plasma and then placing a drop onto a refractometer.
Serum total protein contains albumin and globulins while plasma total protein will also contain fibrinogen and other proteins, so it is important to know what type of sample you have when looking up results. Just remember that serum comes from blood without any anticoagulants added, and plasma comes from blood with anticoagulants such as from "purple-top" tubes which contain a coagulant called EDTA or "green-top tubes" which contain heparin. Also note that some microhematocrit tubes come coated with heparin as an anticoagulant.
Increased total protein may be caused by:
-Dehydration: this is a false or "relative" increase. The amount of protein is actually normal, but the amount of water it is diluted in is decreased. It's like adding a teaspoon of instant coffee to a half a cup of hot water instead of a full cup. The amount of coffee is the same, but the concentration is higher.
-Chronic immune stimulation: either from illness, infection, or immune system disorders.
-Cancer: plasma cell myeloma
Decreased total protein may be caused by:
-Overhydration: as with fluid therapy.
-Liver disease: the liver is responsible for making albumin and many clotting proteins.
-Renal disease: protein loss in the urine.
-GI issues: protein losing enteropathies, exocrine pancreatic insufficiency
-Loss: via internal or external bleeding (even with normal RBC counts due to the reserve of RBC's in the spleen -there is no such reserve for blood proteins and so, this can be a first sign). Proteins may also be lost through exudates such as with severe burns.
-Malnutrition: the body has nothing to make proteins with.
Serum total protein contains albumin and globulins while plasma total protein will also contain fibrinogen and other proteins, so it is important to know what type of sample you have when looking up results. Just remember that serum comes from blood without any anticoagulants added, and plasma comes from blood with anticoagulants such as from "purple-top" tubes which contain a coagulant called EDTA or "green-top tubes" which contain heparin. Also note that some microhematocrit tubes come coated with heparin as an anticoagulant.
Increased total protein may be caused by:
-Dehydration: this is a false or "relative" increase. The amount of protein is actually normal, but the amount of water it is diluted in is decreased. It's like adding a teaspoon of instant coffee to a half a cup of hot water instead of a full cup. The amount of coffee is the same, but the concentration is higher.
-Chronic immune stimulation: either from illness, infection, or immune system disorders.
-Cancer: plasma cell myeloma
Decreased total protein may be caused by:
-Overhydration: as with fluid therapy.
-Liver disease: the liver is responsible for making albumin and many clotting proteins.
-Renal disease: protein loss in the urine.
-GI issues: protein losing enteropathies, exocrine pancreatic insufficiency
-Loss: via internal or external bleeding (even with normal RBC counts due to the reserve of RBC's in the spleen -there is no such reserve for blood proteins and so, this can be a first sign). Proteins may also be lost through exudates such as with severe burns.
-Malnutrition: the body has nothing to make proteins with.
Reading a CBC, Platelets / PLT
Platelets are also called "thrombocytes" and are often counted by machines, but can also be counted on hemocytometers or during manual diffs and then they can be calculated as follows:
(Platelets/100 leukocytes) X (WBC count/mcg) = Platelets/mcg
Here's what a thrombocyte looks like:
Platelets are essential in the body's ability to form a clot when bleeding occurs.
Increased platelets or "thrombocytosis" can be caused by:-Excitement: epinephrine release can cause the number of platelets to increase temporarily.
-Infections
-Inflammation
-Acute or chronic blood loss: the platelets are lost along with the blood.
-Drugs: such as steroids.
-Hyperadrenocorticism: overactive adrenal glands.
-Splenectomy: the spleen is responsible for destroying old platelets which may remain in circulation if the spleen has been removed or is not functioning properly.
-Cancer
-Discontinuation of chemotherapy.
Decreased platelets or "thrombocytopenia" can be caused by:-Decreased production: of platelets by the bone marrow.
-Clotting: the platelets may be used up due to extensive clotting.
-Immune disorder: the immune system may attack its own platelets.
-Sequestration: removal of platelets from the general circulation, possibly due to splenomegaly (an enlarged spleen).
(Platelets/100 leukocytes) X (WBC count/mcg) = Platelets/mcg
Here's what a thrombocyte looks like:
Platelets are essential in the body's ability to form a clot when bleeding occurs.
Increased platelets or "thrombocytosis" can be caused by:-Excitement: epinephrine release can cause the number of platelets to increase temporarily.
-Infections
-Inflammation
-Acute or chronic blood loss: the platelets are lost along with the blood.
-Drugs: such as steroids.
-Hyperadrenocorticism: overactive adrenal glands.
-Splenectomy: the spleen is responsible for destroying old platelets which may remain in circulation if the spleen has been removed or is not functioning properly.
-Cancer
-Discontinuation of chemotherapy.
Decreased platelets or "thrombocytopenia" can be caused by:-Decreased production: of platelets by the bone marrow.
-Clotting: the platelets may be used up due to extensive clotting.
-Immune disorder: the immune system may attack its own platelets.
-Sequestration: removal of platelets from the general circulation, possibly due to splenomegaly (an enlarged spleen).
Friday, August 31, 2012
Reading a CBC, nRBC's / Nucleated RBC's
Nucleated red blood cells are immature RBC's that haven't lost their nucleus yet. These cells are called metarubricytes and look like this:
These immature red blood cells are usually pushed out early in response to anemia, so they indicate regenerative anemia. They are not usually found in normal animals.
Reading a CBC, WBC / NCC / White Blood Cell Count
NCC stands for "Nucleated Cell Count" which works as "White Blood Cell Count" for mammals, but not for birds or reptiles which have nucleated red blood cells.
This is usually a machine-generated number although the total white blood cell count can be done manually with a hemocytometer as well.
White blood cells include neutrophils, lymphocytes, monocytes, eosinophils, and basophils but collectively they are responsible for what we generally think of as immunity. They range from highly specialized cells that go after particular antigens to generalized eaters of our body's "garbage" or stuff like absorbable suture that the body identifies as foreign and, therefore, in need of disposal, or even cells responsible for allergic reactions.
Increases in white blood cells or "leukocytosis" indicates:
-Excitement: this is common in cats. If they become overly excited during the blood draw all of the cells that are normally loosely attached to the endothelial lining of the blood vessels detach and end up in circulation where they can be drawn out and counted. This means that the increase isn't "real" because there aren't really more cells being made, it's just that the ones that aren't usually counted because they stick to the blood vessel wall were counted even though in 30 minutes or so they'll go back to where they belong. If this is the case you'll see normal or slightly increased lymphocyte numbers.
-Inflammation or other causes of neutrophilia: because neutrophils are the most common leukocyte (at least in dogs and cats), when the numbers of neutrophils increase dramatically you can also end up with a leukocytosis as a result.
-Decreases in white blood cells or "leukopenia" indicates:
- Viral diseases: such as feline distemper (aka "panleukopenia"), canine parvovirus, etc
-Infection: bacterial infection, septicemia, toxemia, endotoxins
-Drug-related: such as with the use of sulfonamides
This is usually a machine-generated number although the total white blood cell count can be done manually with a hemocytometer as well.
White blood cells include neutrophils, lymphocytes, monocytes, eosinophils, and basophils but collectively they are responsible for what we generally think of as immunity. They range from highly specialized cells that go after particular antigens to generalized eaters of our body's "garbage" or stuff like absorbable suture that the body identifies as foreign and, therefore, in need of disposal, or even cells responsible for allergic reactions.
Increases in white blood cells or "leukocytosis" indicates:
-Excitement: this is common in cats. If they become overly excited during the blood draw all of the cells that are normally loosely attached to the endothelial lining of the blood vessels detach and end up in circulation where they can be drawn out and counted. This means that the increase isn't "real" because there aren't really more cells being made, it's just that the ones that aren't usually counted because they stick to the blood vessel wall were counted even though in 30 minutes or so they'll go back to where they belong. If this is the case you'll see normal or slightly increased lymphocyte numbers.
-Inflammation or other causes of neutrophilia: because neutrophils are the most common leukocyte (at least in dogs and cats), when the numbers of neutrophils increase dramatically you can also end up with a leukocytosis as a result.
-Decreases in white blood cells or "leukopenia" indicates:
- Viral diseases: such as feline distemper (aka "panleukopenia"), canine parvovirus, etc
-Infection: bacterial infection, septicemia, toxemia, endotoxins
-Drug-related: such as with the use of sulfonamides
Reading a CBC, Basophils
Basophils may be counted by machines or by a technician doing a manual differential or
"manual diff". This involves taking a drop of blood and making a smear
on a slide. It is allowed to dry, then stained with Diff Quick stain.
Once the stain has dried the slide is viewed under a microscope and
evaluated for red and white blood cell morphology as well as a count of
100 white blood cells to determine what percent of cells are of each WBC
type including monocytes.
Basophils are rare. If you see one while looking at a slide, consider yourself lucky. If you hear someone else say they found one, ask to see it. I have yet to see a basophil myself.
Below is a photo of a normal basophil:
Basophils are associated with eosinophils and mast cells, but their use on a CBC is limited due to how rare they are. The causes of their increase are unknown, but usually associated with eosinophilia, or an increase in eosinophils as well.
Basophils are rare. If you see one while looking at a slide, consider yourself lucky. If you hear someone else say they found one, ask to see it. I have yet to see a basophil myself.
Below is a photo of a normal basophil:
Basophils are associated with eosinophils and mast cells, but their use on a CBC is limited due to how rare they are. The causes of their increase are unknown, but usually associated with eosinophilia, or an increase in eosinophils as well.
Reading a CBC, Eosinophils
Eosinophils may be counted by machines or by a technician doing a manual differential or
"manual diff". This involves taking a drop of blood and making a smear
on a slide. It is allowed to dry, then stained with Diff Quick stain.
Once the stain has dried the slide is viewed under a microscope and
evaluated for red and white blood cell morphology as well as a count of
100 white blood cells to determine what percent of cells are of each WBC
type including eosinophils.
The number of eosinophilss may be expressed as a percent or as an absolute number which is expressed as some number per microliter. If you have a choice it is best to work with the absolute number since, with abnormal WBC counts, the number expressed as a percent can be misleading.
Below is a photo of a normal eosinophil although the size of the red granules differ with species, especially the can in which they are more pale and rod-shaped:
Eosinophils are responsible for allergic responses and also play a part in systemic parasite infestations.
Increases in eosinophils or "eosinophilia" occurs as a result of:-Worms: systemic parasites such as heartworm or hookworms.
-Weases: allergic reactions or hypersensitivity reactions including flea bite dermatitis.
-Weird diseases: feline hypereosinophilic syndromes and some poorly characterized gastroenteritis cases.
Decreases in eosinophils or "eosinopenia" occurs as a result of:-Stress: due to increased natural or administered steroids.
The number of eosinophilss may be expressed as a percent or as an absolute number which is expressed as some number per microliter. If you have a choice it is best to work with the absolute number since, with abnormal WBC counts, the number expressed as a percent can be misleading.
Below is a photo of a normal eosinophil although the size of the red granules differ with species, especially the can in which they are more pale and rod-shaped:
Eosinophils are responsible for allergic responses and also play a part in systemic parasite infestations.
Increases in eosinophils or "eosinophilia" occurs as a result of:-Worms: systemic parasites such as heartworm or hookworms.
-Weases: allergic reactions or hypersensitivity reactions including flea bite dermatitis.
-Weird diseases: feline hypereosinophilic syndromes and some poorly characterized gastroenteritis cases.
Decreases in eosinophils or "eosinopenia" occurs as a result of:-Stress: due to increased natural or administered steroids.
Reading a CBC, Monocytes
Monocytes may be counted by machines or by a technician doing a manual differential or
"manual diff". This involves taking a drop of blood and making a smear
on a slide. It is allowed to dry, then stained with Diff Quick stain.
Once the stain has dried the slide is viewed under a microscope and
evaluated for red and white blood cell morphology as well as a count of
100 white blood cells to determine what percent of cells are of each WBC
type including monocytes.
The number of monocytes may be expressed as a percent or as an absolute number which is expressed as some number per microliter. If you have a choice it is best to work with the absolute number since, with abnormal WBC counts, the number expressed as a percent can be misleading.
Below is a photo of a normal monocyte:
Monocytes are the cleanup crew for the body. They migrate out of the blood vessels as needed and then become tissue macrophages, which means they eat dead tissue and anything else that doesn't belong in the body.
Increased monocytes or "monocytosis" is caused by:
-Inflammation: either acute or chronic
-Stress: due to natural or administered steroids, especially in dogs.
Decreased monocytes or "monocytopenia" is caused by:
-Pancytopenia: usually an incidental finding when all white blood cell counts are low which is called "pancytopenia".
The number of monocytes may be expressed as a percent or as an absolute number which is expressed as some number per microliter. If you have a choice it is best to work with the absolute number since, with abnormal WBC counts, the number expressed as a percent can be misleading.
Below is a photo of a normal monocyte:
Monocytes are the cleanup crew for the body. They migrate out of the blood vessels as needed and then become tissue macrophages, which means they eat dead tissue and anything else that doesn't belong in the body.
Increased monocytes or "monocytosis" is caused by:
-Inflammation: either acute or chronic
-Stress: due to natural or administered steroids, especially in dogs.
Decreased monocytes or "monocytopenia" is caused by:
-Pancytopenia: usually an incidental finding when all white blood cell counts are low which is called "pancytopenia".
Reading a CBC, Lymphocytes
Lymphocytes may be counted by machines or by a technician doing a manual differential or
"manual diff". This involves taking a drop of blood and making a smear
on a slide. It is allowed to dry, then stained with Diff Quick stain.
Once the stain has dried the slide is viewed under a microscope and
evaluated for red and white blood cell morphology as well as a count of
100 white blood cells to determine what percent of cells are of each WBC
type including lymphocytes, which are the most common white blood cells in cattle.
The number of lymphocytes may be expressed as a percent or as an absolute number which is expressed as some number per microliter. If you have a choice it is best to work with the absolute number since, with abnormal WBC counts, the number expressed as a percent can be misleading.
Below is a photo of 2 normal lymphocytes:
Lymphocytes include the cells responsible for both humoral and cell-mediated immunity. Sometimes they may appear with blue cytoplasm, these are reactive forms which are likely B cells.
Increased lymphocytes or "lymphocytosis" is caused by:
-Excitement: this is common in cats. If they become overly excited during the blood draw all of the cells that are normally loosely attached to the endothelial lining of the blood vessels detach and end up in circulation where they can be drawn out and counted. This means that the increase isn't "real" because there aren't really more cells being made, it's just that the ones that aren't usually counted because they stick to the blood vessel wall were counted even though in 30 minutes or so they'll go back to where they belong. If this is the case you'll see increased numbers of neutrophils as well (neutrophilia).
-Leukemia
Decreased lymphocytes or "lymphocytopenia" is caused by:
-Stress: an increase in steroids which can also be due to the administration of steroids
-Acute viral infection: usually accompanied by beutropenia or a decrease in neutrophils as well.
The number of lymphocytes may be expressed as a percent or as an absolute number which is expressed as some number per microliter. If you have a choice it is best to work with the absolute number since, with abnormal WBC counts, the number expressed as a percent can be misleading.
Below is a photo of 2 normal lymphocytes:
Lymphocytes include the cells responsible for both humoral and cell-mediated immunity. Sometimes they may appear with blue cytoplasm, these are reactive forms which are likely B cells.
Increased lymphocytes or "lymphocytosis" is caused by:
-Excitement: this is common in cats. If they become overly excited during the blood draw all of the cells that are normally loosely attached to the endothelial lining of the blood vessels detach and end up in circulation where they can be drawn out and counted. This means that the increase isn't "real" because there aren't really more cells being made, it's just that the ones that aren't usually counted because they stick to the blood vessel wall were counted even though in 30 minutes or so they'll go back to where they belong. If this is the case you'll see increased numbers of neutrophils as well (neutrophilia).
-Leukemia
Decreased lymphocytes or "lymphocytopenia" is caused by:
-Stress: an increase in steroids which can also be due to the administration of steroids
-Acute viral infection: usually accompanied by beutropenia or a decrease in neutrophils as well.
Reading a CBC, Segs / Neutrophils
Neutrophils may be counted by machines or by a technician doing a manual differential or
"manual diff". This involves taking a drop of blood and making a smear
on a slide. It is allowed to dry, then stained with Diff Quick stain.
Once the stain has dried the slide is viewed under a microscope and
evaluated for red and white blood cell morphology as well as a count of
100 white blood cells to determine what percent of cells are of each WBC
type including neutrophils, which are the most common white blood cells in dogs and cats.
The number of neutrophils may be expressed as a percent or as an absolute number which is expressed as some number per microliter. If you have a choice it is best to work with the absolute number since, with abnormal WBC counts, the number expressed as a percent can be misleading.
Below is a photo of a normal, mature, segmented neutrophil:
Neutrophils are the body's first line of defense against infection and also play a part in inflammation.
Increased neutrophils is called "neutrophilia" and may indicate:
-Inflammation: if this is the case it is often accompanied by a left shift.
-Stress: caused by an increase of steroids including those used as medication and usually indicated by a decrease in lymphocytes aka "lymphocytopenia".
-Excitement: this is common in cats. If they become overly excited during the blood draw all of the cells that are normally loosely attached to the endothelial lining of the blood vessels detach and end up in circulation where they can be drawn out and counted. This means that the increase isn't "real" because there aren't really more cells being made, it's just that the ones that aren't usually counted because they stick to the blood vessel wall were counted even though in 30 minutes or so they'll go back to where they belong. If this is the case you'll see normal or slightly increased lymphocyte numbers.
Decreased neutrophils is called "neutropenia" and may indicate:
-Inflammation: usually accompanied by a left shift.
-Infection: especially viruses such as parvovirus. In this case other blood cell numbers will also go down in the order of their circulating lifespan.
-Bone marrow suppression: due to illness or drugs such as estrogen, chemotherapy, ehrlichiosis
The number of neutrophils may be expressed as a percent or as an absolute number which is expressed as some number per microliter. If you have a choice it is best to work with the absolute number since, with abnormal WBC counts, the number expressed as a percent can be misleading.
Below is a photo of a normal, mature, segmented neutrophil:
Neutrophils are the body's first line of defense against infection and also play a part in inflammation.
Increased neutrophils is called "neutrophilia" and may indicate:
-Inflammation: if this is the case it is often accompanied by a left shift.
-Stress: caused by an increase of steroids including those used as medication and usually indicated by a decrease in lymphocytes aka "lymphocytopenia".
-Excitement: this is common in cats. If they become overly excited during the blood draw all of the cells that are normally loosely attached to the endothelial lining of the blood vessels detach and end up in circulation where they can be drawn out and counted. This means that the increase isn't "real" because there aren't really more cells being made, it's just that the ones that aren't usually counted because they stick to the blood vessel wall were counted even though in 30 minutes or so they'll go back to where they belong. If this is the case you'll see normal or slightly increased lymphocyte numbers.
Decreased neutrophils is called "neutropenia" and may indicate:
-Inflammation: usually accompanied by a left shift.
-Infection: especially viruses such as parvovirus. In this case other blood cell numbers will also go down in the order of their circulating lifespan.
-Bone marrow suppression: due to illness or drugs such as estrogen, chemotherapy, ehrlichiosis
Reading a CBC, Bands
Machines cannot reliably distinguish between band neutrophils and mature neutrophils yet (although they are very close), so this value is usually determined by a technician doing a manual differential or "manual diff". This involves taking a drop of blood and making a smear on a slide. It is allowed to dry, then stained with Diff Quick stain. Once the stain has dried the slide is viewed under a microscope and evaluated for red and white blood cell morphology as well as a count of 100 white blood cells to determine what percent of cells are of each WBC type including bands.
Bands are immature neutrophils. In the photo below, the white blood cell on the left is a band neutrophil while the one on the right is a "Seg" or normal, mature, segmented neutrophil:
Immature "band" neutrophils are released from the bone marrow when the body is running low on circulating, mature, neutrophils and decides that immature cells are better than none at all. Neutrophils are the body's first line of defense against infection, but they are also involved in inflammation. So, whichever the cause, band neutrophils indicate that the body's normal defenses aren't able to keep up.
When bands are present it's called a "left shift". The next question to ask yourself is whether there are more bands or more mature neutrophils present. If there are more mature neutrophils than bands it is a better prognosis and it's called a "regenerative left shift". This means that bands are being produced, but the body is still putting up a good fight. If there are more bands than segs, it's called a "degenerative left shift". This is a bad prognosis because it indicates the body is not keeping up -it is losing the battle.
The presence of bands indicates:
-Inflammation: this is the most common cause.
-Bone marrow disorders such as leukemia may cause early release of neutrophils.
-Bone marrow injury
The absence of bands indicates:-Normal, yay!
Bands are immature neutrophils. In the photo below, the white blood cell on the left is a band neutrophil while the one on the right is a "Seg" or normal, mature, segmented neutrophil:
Immature "band" neutrophils are released from the bone marrow when the body is running low on circulating, mature, neutrophils and decides that immature cells are better than none at all. Neutrophils are the body's first line of defense against infection, but they are also involved in inflammation. So, whichever the cause, band neutrophils indicate that the body's normal defenses aren't able to keep up.
When bands are present it's called a "left shift". The next question to ask yourself is whether there are more bands or more mature neutrophils present. If there are more mature neutrophils than bands it is a better prognosis and it's called a "regenerative left shift". This means that bands are being produced, but the body is still putting up a good fight. If there are more bands than segs, it's called a "degenerative left shift". This is a bad prognosis because it indicates the body is not keeping up -it is losing the battle.
The presence of bands indicates:
-Inflammation: this is the most common cause.
-Bone marrow disorders such as leukemia may cause early release of neutrophils.
-Bone marrow injury
The absence of bands indicates:-Normal, yay!
Reading a CBC, Reticulocytes
Reticulocytes are young red blood cells. If viewed on a slide with Diff Quick stain they'd be called polychromatophils because they'd appear larger than the RBC's and slightly bluish in color. When viewed on a slide using New Methylene Blue stain they appear as large RBC's with one or more dark purplish dots inside. These are the remnants of the nucleus which is not quite gone because of the cells immaturity. The image below is of reticulocytes stained with New Methylene Blue:
If reticulocytes are present it may indicate:
-regenerative anemia
If reticulocytes are not present it is:
-normal! Yay!
If reticulocytes are present it may indicate:
-regenerative anemia
If reticulocytes are not present it is:
-normal! Yay!
Reading a CBC, MCHC / Mean Corpuscular Hemoglobin Concentration
MCHC or Mean Corpuscular Hemoglobin Concentration is the average amount of hemoglobin in the red blood cells. It is usually a machine-determined value, but it can be estimated like this:
MCHC = (Hb / PCV) X 100
Increased MCHC:
-Machine error: there is no such thing as hyperchromic RBC's
Decreased MCHC:-Regenerative anemia: immature cells have less hemoglobin than mature cells, so a low MCHC can indicate regenerative anemia. MCV, reticulocytes, and nRBC's should also be looked at as well to confirm that the cause of the low MCHC is regenerative anemia.
MCHC = (Hb / PCV) X 100
Increased MCHC:
-Machine error: there is no such thing as hyperchromic RBC's
Decreased MCHC:-Regenerative anemia: immature cells have less hemoglobin than mature cells, so a low MCHC can indicate regenerative anemia. MCV, reticulocytes, and nRBC's should also be looked at as well to confirm that the cause of the low MCHC is regenerative anemia.
Reading a CBC, MCV or Mean Corpuscular Volume
MCV stands for Mean Corpuscular Volume. In plain English that's the average size of the red blood cells. It is usually determined by machine, but can be calculated manually like this:
MCV = (PCV / RBC count) X 10.
Increased MCV or "macrocytosis" may be due to:
-Regenerative anemia: Immature RBC's are larger than mature RBC's, so a high MCV is one indicator of regenerative anemia although reticulocytes and nRBC's should also be looked at.
-Clumped platelets: Clumps of platelets may be counted as RBC's by the CBC machine. If this is suspected a slide should be made from the same blood sample that was used to run the CBC in order to check for clumped platelets.
Decreased MCV or "microcytosis" may be due to:
-Extreme spherocytosis: Usually spherocytosis does not result in a decreased MCV, but in extreme cases it can.
MCV = (PCV / RBC count) X 10.
Increased MCV or "macrocytosis" may be due to:
-Regenerative anemia: Immature RBC's are larger than mature RBC's, so a high MCV is one indicator of regenerative anemia although reticulocytes and nRBC's should also be looked at.
-Clumped platelets: Clumps of platelets may be counted as RBC's by the CBC machine. If this is suspected a slide should be made from the same blood sample that was used to run the CBC in order to check for clumped platelets.
Decreased MCV or "microcytosis" may be due to:
-Extreme spherocytosis: Usually spherocytosis does not result in a decreased MCV, but in extreme cases it can.
Reading a CBC, Hgb / Hb / Hemoglobin
Hemoglobin is often abbreviated Hgb or Hb, either way it is the measurement of the oxygen-carrying component of the red blood cells. This number should be pretty close to being equal to the PCV divided by 3. I remember this because it rhymes: "Hb equals PCV over 3". This value is determined by the CBC machine.
Increased hemoglobin indicates:
-Machine error: there is no such thing as a real increase of hemoglobin.
Decreased hemoglobin indicates:
-Regenerative anemia: young RBC's don't have as much hemoglobin as mature cells. See MCV, reticulocytes, and NRBC's to confirm.
Increased hemoglobin indicates:
-Machine error: there is no such thing as a real increase of hemoglobin.
Decreased hemoglobin indicates:
-Regenerative anemia: young RBC's don't have as much hemoglobin as mature cells. See MCV, reticulocytes, and NRBC's to confirm.
Reading a CBC: RBC / Red Blood Cell Count
The Red Blood Cell Count is given by a CBC machine and tells you the number of RBC's in a microliter of blood. This number should be compared to the PCV since they both are giving you an idea of the number of red blood cells in the blood.
Increased RBC count may be caused by:
-Platelet clumping: platelet clumps are often read by machines as being RBC's. If there are a lot of clumps it could throw your RBC count off by quite a bit. Compare to your PCV and check your MCV to determine if this is the case.
-Dehydration: check the albumin, if it is also high dehydration is likely.
Decreased RBC count may be caused by:
A decreased RBC count indicates anemia which has 3 main causes:
-Lack of RBC production: from bone marrow issues, nutrition problems, or kidney problems since the kidneys stimulate production via erythropoietin.
-Increased RBC destruction: due to intracellular parasites, immune disorders (IMHA), etc
-Loss: from external or internal bleeding.
Increased RBC count may be caused by:
-Platelet clumping: platelet clumps are often read by machines as being RBC's. If there are a lot of clumps it could throw your RBC count off by quite a bit. Compare to your PCV and check your MCV to determine if this is the case.
-Dehydration: check the albumin, if it is also high dehydration is likely.
Decreased RBC count may be caused by:
A decreased RBC count indicates anemia which has 3 main causes:
-Lack of RBC production: from bone marrow issues, nutrition problems, or kidney problems since the kidneys stimulate production via erythropoietin.
-Increased RBC destruction: due to intracellular parasites, immune disorders (IMHA), etc
-Loss: from external or internal bleeding.
Reading a CBC, PCV / HCT
PCV is the Packed Cell Volume which is also known as the hematocrit or HCT. Generally this is determined by taking a microhematocrit tube, filling it with blood collected in a tube, plugging one end with clay, and then spinning it at very high speeds in a centrifuge. After spinning, the blood components will separate in the tube with the red blood cells on the bottom, the white blood cells on top of that, and the plasma at the very top. The hematocrit tube is then placed on a reading card as shown below with the top of the clay lined up with the bottom line and the top of the plasma lined up with the top line. Finally, you find the number that matches up with the top of the red blood cells in the tube. So, in the picture below, if the red lines indicate changes of 10% on the table, the PCV of that hematocrit tube would be about 50%.
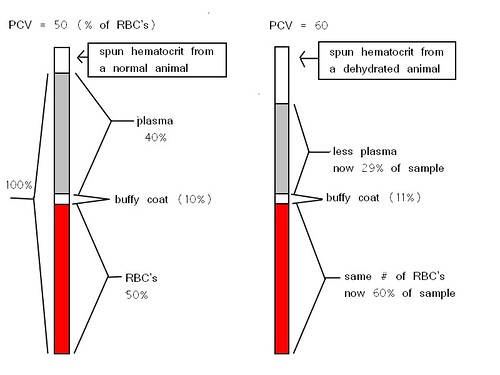
It is important to keep in mind that what this test really measures is the percent of the blood that is made up of red blood cells. The PCV is expected to go down in cases of anemia, but go up in cases of dehydration since there is less water (plasma) but the same number of RBC's. The drawing below may make the change with dehydration more clear. Click on it if you need to see a larger version of the image.
Decreased PCV:
A lower than normal PCV indicates anemia which has 3 main causes:
-Lack of RBC production: from bone marrow issues, nutrition problems, or kidney problems since the kidneys stimulate production via erythropoietin.
-Increased RBC destruction: due to intracellular parasites, immune disorders (IMHA), etc
-Loss: from external or internal bleeding.
Increased PCV:
-Dehydration: this is most common, but it is important to look at the albumin results of the Chemistry test and compare it to the PCV. If both are high the cause is likely dehydration.
Subscribe to:
Posts (Atom)
