Pharmacy math is often intimidating, but it is really important that we
get it right, so here's a little post aimed at making you more
comfortable doing compounding math.
1. Make 10ml of Methimazole with 5mg tablets at 5mg/ml.
We need 10ml at 5mg/ml. That's 5mg for every ml.
So, if we want 10ml, we multiply top and bottom by 10.
That's 5mg X 10 = 50mg in 1ml X 10 =10ml.
We need 50mg of Methimazole and our Methimazole is in 5mg tablets.
So we divide 50mg by 5mg to get the number of tablets we need:
50 / 5 = 10. We need 10 tablets.
And our total volume is 10ml, so we need 10 tablets in 10ml of solution.
2. Make 30ml of Doxy from 50mg capsules at 25mg/ml.
We need 30ml at 25mg/ml. So, multiply the top and bottom by 30:
25mg X 30 = 750mg. 1ml X 30 =30ml
So we need750mg of Doxy in 30ml of solution.
Since our Doxy is 50mg we need to know how many capsules to use to gt 750mg:
750mg/50mg capsules = 15 capsules
So, we need to use 15 capsules and 30ml of solution.
3. Make 20ml of 15mg/ml Meloxicam from 7.5mg tablets.
We need 20ml at 15mg/ml. So, multiply the top and bottom by 20:
15mg X 20 = 300mg. 1ml X 20 = 20ml
We need 300mg and we have 7.5mg tablets, so:
300mg/7.5mg tablets = 40 tablets in 20ml of solution.
4. Make 12ml of 25mg/ml Baytril from 100mg/ml (injectable) Baytril.
This is a little different since our medication is liquid. In the above
problems our total volume and amount of solution needed were always the
same, but for liquid medications the medication's volume has to be
taken into account as part of the final solution, so we need to use the
formula:
(C1) X (V1) = (C2) X (V2)
Original concentration (C1) = 100mg/ml Baytril
Original volume (V1) = unknown amount of Baytril
Final concentration (C2) = 25mg/ml Baytril
Final volume (V2) = 12ml of solution
So: 100 X (x) = 25 X 12
Multiply each side to get: 100x = 300
Solve for x: 300/100 = x, so x = 3
So, we need 3ml of Baytril.
And we need 12ml total.
So, 3ml Baytril and the rest of the volume will be solution.
Find the amount of solution by subtracting the amount of Baytril from the total volume:
12ml total - 3m Baytril = 9ml of solution
5. Make 4ml of 10mg/ml Baytril from 100mg/ml (injectable) Baytril.
4 X 10mg = 40mg
4 X 1ml = 4ml
C1 = 100mg/ml Baytril
V2 = unknown amount of Baytril
C2 = 10mg/ml Baytril
V2 = 4ml
100 X ? = 10 X 4
100X = 40
X = 40/100
X = 0.4
0.4ml Baytril
Total solution = 4ml
4ml total = 0.4ml Baytril means 3.6ml of solution will be used.
Information for Vet Techs and Vet Assistants as well as cool cases to share and discuss.
Tuesday, September 17, 2013
Thursday, August 8, 2013
Evaluating a blood smear
1. Make a blood smear and stain it. For a refresher on how to do this, check out this video:
http://www.youtube.com/watch?v=R1DU_N6eazg
2. Put the slide on the microscope and focus using low power magnification, then move up to high dry.
3. On high dry magnification, briefly scan the slide to find where your monolayer is. The monolayer is where you'd do your cell counts -the area where the cells do not overlap, but cover the whole viewing area without many gaps. Then find the feathered edge where the cells are more spread out at the end of your smear. Evaluate whether there are more white blood cells at the edge than the monolayer or not. If there are, this may erroneously decrease your white blood cell count and another smear should be made.
4. Move up to oil power and then scan the feathered edge for platelets. Again, if there seem to be a lot of platelets or clumped platelets at the feathered edge this will erroneously decrease your platelet count and another smear should be made.
5. If everything looks okay, move to your monolayer and begin your evaluation.
Things to look for by type:
http://www.youtube.com/watch?v=R1DU_N6eazg
2. Put the slide on the microscope and focus using low power magnification, then move up to high dry.
3. On high dry magnification, briefly scan the slide to find where your monolayer is. The monolayer is where you'd do your cell counts -the area where the cells do not overlap, but cover the whole viewing area without many gaps. Then find the feathered edge where the cells are more spread out at the end of your smear. Evaluate whether there are more white blood cells at the edge than the monolayer or not. If there are, this may erroneously decrease your white blood cell count and another smear should be made.
4. Move up to oil power and then scan the feathered edge for platelets. Again, if there seem to be a lot of platelets or clumped platelets at the feathered edge this will erroneously decrease your platelet count and another smear should be made.
5. If everything looks okay, move to your monolayer and begin your evaluation.
Things to look for by type:
- White blood cells (in order of prevalence in dogs and cats):
- Neutrophils:
- Segments: Neutrophils should have 4-5 segments on average. They may appear to have fewer due to their being viewed in 2D. When a good percentage of neutrophils have more than 5 segments indicates hypersegmentation or older neutrophils that may be kept around longer due to decreased production as happens with steroid use. Consistantly seeing hyposegmented neutrophils (or neutrophils with fewer than 4 segments) may indicate younger than average neutrophils as happens at the beginning or end of a left shift. A neutrophil with a nucleus that has parallel sides for its entire length (no segments) is called a "band" and seeing many bands in a smear indicates a "left shift". If under 50% of neutrophils are bands the left shift is regenerative. If over 50% of the neutrophils are bands the left shift is degenerative.
- Signs of toxicity: Dohle bodies appear as dark spots in the cytoplasm. Vacuoles look like "bubbles" or white spots in the cytoplasm. Blue or "basophilic" cytoplasm, or more noticeable granules in the cytoplasm (toxic granulation).
- Lymphocytes:
- Abnormal findings: Red granules in the cytoplasm of more than a few cells can indicate Ehrlichia canis infection or cancer.. Lymphs with deeper blue cytoplasm are reactive lymphocytes and can be normal in young animals.
- Monocytes:
- Distinct from lymphocytes due to their large size and vacuoles as well as their less dense nucleus and larger amount of cytoplasm surrounding the nucleus.
- Eosinophils:
- Segments: Should be evaluated the same as neutrophils although they may be difficult to see due to the visible granules.
- Basophils:
- Very rare to see.
- Segments: Should be evaluated the same as neutrophils although they may be difficult to see due to the visible granules. No link provided because Cornell's basophil photo is very poor.
- Red Blood Cells:
- Cell size: If the cells differ in size, this is called anisocytosis.
- Cell color: Large cells that are more blue are called "polychromatophils" and are not quite mature. Pale cells are called "hypochromic". Clear cells are called "ghost cells" and indicate that the cell membrane had a leak.
- Shape: If an RBC has a knob or an "ear" or "nose" growing out of it, this is likely a Heinz body. RBC's that look like splats may be acanthocytes or echinocytes. Acanthocytes have irregular protrusions that may be round on the ends while echinocytes have a pointier protrusions all over the cell. Target cells look like targets in that they have an area of central pallor with a circle of red inside of it. If it looks like a red blood cell was ripped and you are just seeing a piece of it the piece is called a schistocyte. Teardrop shaped RBC's are dacryocytes and are usually an artifact from making the smear. Spherocytes are smaller RBC's with no area of central pallor. A general term for differently shaped red blood cells is poikilocytosis.
- Inclusions: Large dark circles that make the RBC look like a googly eye or a fried egg are early stage cells that still have their nucleus, these are called metarubricytes. Smaller dots in the red blood cell are Howell Jolly bodies if they are not refractile (shiny when the focus is moved up and down). If they are refractile they are likely granules from the stain. Real Howell Jolly bodies often occur between the center of the cell and the membrane rather than right in the center or touching the membrane. Basophilic stippling appears as lots of granular looking dots and can mean resolving anemia or lead poisoning. RBC parasites may also be seen. Check the menu on the left of this page for more about these: https://ahdc.vet.cornell.edu/clinpath/modules/rbcmorph/para-f.htm
- Platelets:
- Platelets appear as irregularly shaped basophilic cells that are usually smaller than a red blood cell. If you are in the monolayer and you are seeing 10-15 platelets per oil field you can assume the platelet count is average. If you are unsure or are asked to do a platelet count than count the number of platelets per oil power field across 10 fields and then average them. Multiply the average by 15,000 and you'll get an estimated platelet count per microliter. Normal platelet counts should close to or above 200,000 per microliter.
- For basic manual differentials: Evaluate as many fields in the monolayer as necessary to count 100 white blood cells by type. At the end the number of each cell type gives you the percentage of that cell in the smear. For example, 64 neutrophils, 26 lymphs, 7 monocytes, and 3 eosinophils means there are 64% neutrophils, 26% lymphs, 7% monocytes, and 3% eos. But, you should also be taking note of any irregularities in the WBC's or the RBC's and should take a mental note of the platelet numbers you are seeing by field as well. If nothing seems out of the ordinary just give the cell percentages, but if anything abnormal was found it should be reported.
- For patients who are anemic: A platelet count is usually what is asked for. In addition to the platelet count the RBC's should be evaluated fully. This can give the doctor a hint as to what the problem might be or an idea of whether or not the anemia is regenerative or not (whether the animal is creating new RBC's and then losing them or if the issue might be that they have stopped producing them).
- Heartworm microfilaria: Examine the smear on low or medium power. The microfilaria are longer than 50 RBC's strung together, so they should be pretty obvious if present.
Sunday, June 23, 2013
Work Journal -June 23, 2013 Euthanasia
When asked the "what do you do for a living?" question my reply is
usually met with the response that "euthanasias must be so hard". In
reality, most pets are euthanized for good cause and it is much harder
emotionally when an owner can't make the decision to end their pet's
suffering.
Today a stability check was called for a dog that "wasn't doing well in the lobby" and when I ran to go get it I was met with a receptionist running towards treatment with the dog. I helped open the door for her and grabbed the oxygen as she laid it on the table. As I placed the mask over the dog's mouth the receptionist began to tell me the patient's history. He had a history of CHF (Congestive Heart Failure) for the last 3 years, well managed with medication, then acutely had trouble breathing and wet sounding respirations this morning.
The dog was given a dose of furosamide and then the doctor left to talk to the owner. Upon her return I reported that the dogs color was getting worse and his RR had nearly doubled. But, I was told the owner wasn't prepared to euthanize and had to think it over. The doctor attempted to suck out some of the pinkish foam that was gathering in the dog's pharynx to allow him to breathe better and when it was clear that it wasn't really helping she left again to tell the owner that the dog was going downhill pretty fast.
And, as the owner weighed the decision, I was left standing there with this bug-eyed dog who was fighting for air. At first he was making up for his fluid filled lungs by simply breathing faster. This allowed the tiny portion of his lungs that weren't drowning in fluid to exchange enough oxygen to keep him alive and pink at first. But by the time the doctor came back from talking to the owner the dog's color was muddy and he was trying to sit up in an effort to allow his lungs to expand just a little further. After the doctor left the second time the dog started to fight the oxygen mask. He was panicking as he was drowning due to the fluid in his chest. He tried standing several times, but the increased effort caused him to breathe even harder and faster with each attempt. I tried to calm him, tried to hold him up so he could expand his chest without using extra energy to stand. I tried to deliver the oxygen in any way I could think of to reduce his stress, and tried to talk to him, pet him, keep him warm. But the whole time I kept staring at the real solution -the euthanasia solution in the syringe one foot away. Because I knew there was no winning this fight. All that could be hoped for was a peaceful end -soon.
And it eventually happened. He just went limp in my arms and seized as his heart gave up. In the end the owner didn't have to make the decision that she dreaded so much. I cleaned him up and carried him in for her to say goodbye and she got to skip seeing him panicked and fighting for air for who knows how long. I don't blame her for her hesitation, though. I know firsthand that giving the okay to euthanize feels like you, yourself, are killing your friend, your family member. But as one who spends those last precious moments with many terminal patients I can say that euthanasia is not something I fear. In fact it is sometimes something that I sometimes wish for desperately.
Today a stability check was called for a dog that "wasn't doing well in the lobby" and when I ran to go get it I was met with a receptionist running towards treatment with the dog. I helped open the door for her and grabbed the oxygen as she laid it on the table. As I placed the mask over the dog's mouth the receptionist began to tell me the patient's history. He had a history of CHF (Congestive Heart Failure) for the last 3 years, well managed with medication, then acutely had trouble breathing and wet sounding respirations this morning.
The dog was given a dose of furosamide and then the doctor left to talk to the owner. Upon her return I reported that the dogs color was getting worse and his RR had nearly doubled. But, I was told the owner wasn't prepared to euthanize and had to think it over. The doctor attempted to suck out some of the pinkish foam that was gathering in the dog's pharynx to allow him to breathe better and when it was clear that it wasn't really helping she left again to tell the owner that the dog was going downhill pretty fast.
And, as the owner weighed the decision, I was left standing there with this bug-eyed dog who was fighting for air. At first he was making up for his fluid filled lungs by simply breathing faster. This allowed the tiny portion of his lungs that weren't drowning in fluid to exchange enough oxygen to keep him alive and pink at first. But by the time the doctor came back from talking to the owner the dog's color was muddy and he was trying to sit up in an effort to allow his lungs to expand just a little further. After the doctor left the second time the dog started to fight the oxygen mask. He was panicking as he was drowning due to the fluid in his chest. He tried standing several times, but the increased effort caused him to breathe even harder and faster with each attempt. I tried to calm him, tried to hold him up so he could expand his chest without using extra energy to stand. I tried to deliver the oxygen in any way I could think of to reduce his stress, and tried to talk to him, pet him, keep him warm. But the whole time I kept staring at the real solution -the euthanasia solution in the syringe one foot away. Because I knew there was no winning this fight. All that could be hoped for was a peaceful end -soon.
And it eventually happened. He just went limp in my arms and seized as his heart gave up. In the end the owner didn't have to make the decision that she dreaded so much. I cleaned him up and carried him in for her to say goodbye and she got to skip seeing him panicked and fighting for air for who knows how long. I don't blame her for her hesitation, though. I know firsthand that giving the okay to euthanize feels like you, yourself, are killing your friend, your family member. But as one who spends those last precious moments with many terminal patients I can say that euthanasia is not something I fear. In fact it is sometimes something that I sometimes wish for desperately.
Friday, June 21, 2013
Work Journal: May 23, 2013 Lessons we learned from a dead hamster.
Two techs and a
doctor stand leaning over a table at a dying hamster. The owner had
said goodbye and the euthanasia solution had been injected out of sight
in the treatment area due to the lack of accessible veins in such small
"pocket pets". The heartbeat was down to about 20 Bpm, but we were all
patiently waiting for zero.
The hamster had an obvious abdominal mass that we all wanted to explore and understand, but no poking or prodding was being done because none of us wanted to cause any pain or discomfort to an animal who had already suffered for some time.
Those of us into veterinary medicine do so because of two things: we care about animals, and we are interested in medicine. But, clearly the animal comes first.
So, then the thought crosses my mind that you can still find people today, and the majority of people a few decades ago thought animals were incapable of feeling pain. But here we are, quiet, patient, one of us holding the tiny hamster's hand as we talk about what the mass might be and how sad the adult owner was and what an awesome hammy he must have been to made such an impact.
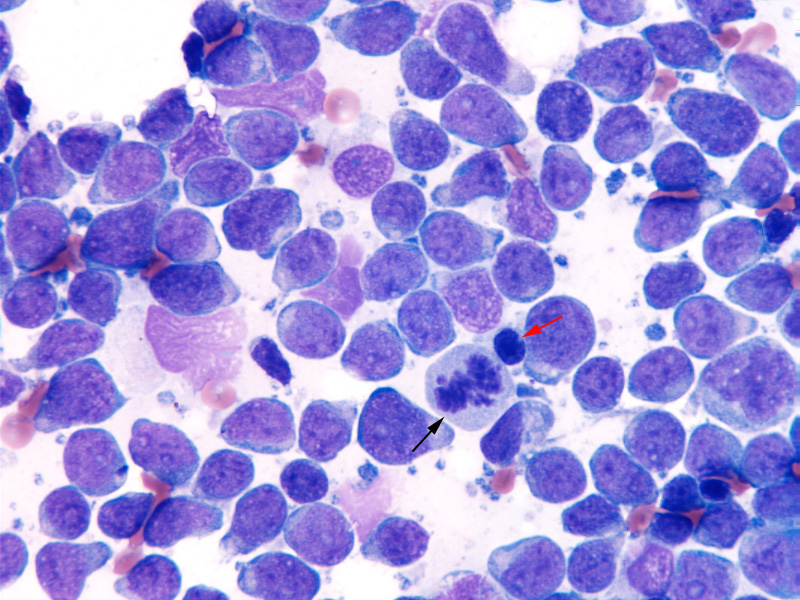
When the doctor felt he was gone she passed the stethoscope to me to double-check. I agreed that no heartbeat was present and handed the stethoscope to the other tech to triple check. Only when we had all agreed that the hamster was gone did we begin to feel the mass and other internal organs to make our guesses. When everyone had finished palpating I took an aspirate of the mass to look at under the microscope and discovered that it was likely a large cell lymphoma which the doctor's reference book said was common for hamsters.
Similar photo of the aspirate under the microscope:
The hamster had an obvious abdominal mass that we all wanted to explore and understand, but no poking or prodding was being done because none of us wanted to cause any pain or discomfort to an animal who had already suffered for some time.
Those of us into veterinary medicine do so because of two things: we care about animals, and we are interested in medicine. But, clearly the animal comes first.
So, then the thought crosses my mind that you can still find people today, and the majority of people a few decades ago thought animals were incapable of feeling pain. But here we are, quiet, patient, one of us holding the tiny hamster's hand as we talk about what the mass might be and how sad the adult owner was and what an awesome hammy he must have been to made such an impact.
When the doctor felt he was gone she passed the stethoscope to me to double-check. I agreed that no heartbeat was present and handed the stethoscope to the other tech to triple check. Only when we had all agreed that the hamster was gone did we begin to feel the mass and other internal organs to make our guesses. When everyone had finished palpating I took an aspirate of the mass to look at under the microscope and discovered that it was likely a large cell lymphoma which the doctor's reference book said was common for hamsters.
Similar photo of the aspirate under the microscope:
Sunday, May 19, 2013
Work Journal May 19, 2013
5/18/2013: "Stability check -its an emergency!". As we looked at
each other with a "this must be bad" look a man in spandex ran in
carrying a dog. We had gotten oxygen hooked up at that point, so I ran
for a mask as the Dr asked him "can you briefly tell me what happened?"
while my fellow techs grabbed the emergency drugs and intubation
supplies. The man responded "I left him in the car while I went for a
hike, I guess it was too hot". He was then led from the room by a CSR
while the Dr started CPR with me giving breaths via the anesthetic
machine's breathing bag. Finally a thermometer beeped and gave us the
news -he was too hot to register, over 115*F. Within minutes he was
dark purple, CPR was not working, so the Dr called us off of him. The
doctor notifed the owner and asked if he wanted to visit with the dog,
he refused, paid for cremation, and left. UPDATE: We got news that
this man was arrested for charges related to this event. Something to
note about this case is that it was in the low 70's in Oakland that day.
It doesn't take super hot weather for temperatures in a car to rise
high enough to kill. ...and what a horrible way to
die!
5/19/2013: "Stability check on a stray dog who can't walk". A fellow tech went to get the dog and brought it back. It was a middle aged female bull terrier -her feet were swollen to twice their normal size and the skin was badly infected (visible puss between the toes) -you could smell her from across the room! The nails on several toes had grown in full circles and embedded themselves in her paw pads. The skin on her inner thighs was crusted with purulent material and raw. Once cleaned we could see that much of the skin had cracked and opened up exposing the red dermis below. She had puncture wounds on her shoulder, hip, and feet, she was thin and had the muscles of her head had wasted away. She was also dehydrated. The people who found her were asked if they wanted to take responsibility for her -a question that is often answered "no" because it hits people in the pocketbook and her condition was bad enough that the hit was likely to be pretty substancial. But, the people said yes, so an IVC was placed and fluids were started, we soaked her feet in dilute chlorhex solution, trimmed the nails, and cleaned her feet and wounds as best we could without stressing her out too much. At the end of the night her new owners came to pick her up and take her to her new home for the night -she'll be returning tomorrow morning for further care
5/19/2013: "Stability check on a cat, it's an emergency!". We really didn't want to hear those words ever again much less again the very next day. I ran to go get it and it turned out to be a cat in a cardboard box. It was open a little and I could see a large (1cm) puncture above the right eye that looked old and the cat was covered in dirt and pine needles. (It seriously looked like it just clawed its way out of the Pet Cemetary.) I asked if the people know what happened and they said she "must have been beat up pretty bad" and added that it was a neighborhood cat. Awesome. So, I brought it in back where the other techs had set up oxygen and the crash kit and I opened the box. All I could see was the entire box and the cat moving as if I was seeing a TV station that wasn't coming in clearly. The cat wasn't moving, everything in the box was. Once my brain made sense of what I was seeing I realized there were ants everywhere. Next, I realized they were crawling out of the wound I had seen earlier. She turned out to have over 10 pucture wounds all over her face and neck that were necrotic and infested with ants and maggots. She also had a deep necrotic wound on her foot. We got word that the people who brought her in approved charges into the thousands of dollars, but the doctor convinced them that euthanisia was the most humane option.
5/19/2013: There were so many stability checks today that only 1 tech and 0 doctors got lunch. VCA provided pizza around 1pm. I finally got a slice around 5pm. A full day, but I prefer that to standing around doing nothing. I also got to participate in another large surgery today for more practice (an exploratory that also ended in euthanasia).
5/19/2013: "Stability check on a stray dog who can't walk". A fellow tech went to get the dog and brought it back. It was a middle aged female bull terrier -her feet were swollen to twice their normal size and the skin was badly infected (visible puss between the toes) -you could smell her from across the room! The nails on several toes had grown in full circles and embedded themselves in her paw pads. The skin on her inner thighs was crusted with purulent material and raw. Once cleaned we could see that much of the skin had cracked and opened up exposing the red dermis below. She had puncture wounds on her shoulder, hip, and feet, she was thin and had the muscles of her head had wasted away. She was also dehydrated. The people who found her were asked if they wanted to take responsibility for her -a question that is often answered "no" because it hits people in the pocketbook and her condition was bad enough that the hit was likely to be pretty substancial. But, the people said yes, so an IVC was placed and fluids were started, we soaked her feet in dilute chlorhex solution, trimmed the nails, and cleaned her feet and wounds as best we could without stressing her out too much. At the end of the night her new owners came to pick her up and take her to her new home for the night -she'll be returning tomorrow morning for further care
5/19/2013: "Stability check on a cat, it's an emergency!". We really didn't want to hear those words ever again much less again the very next day. I ran to go get it and it turned out to be a cat in a cardboard box. It was open a little and I could see a large (1cm) puncture above the right eye that looked old and the cat was covered in dirt and pine needles. (It seriously looked like it just clawed its way out of the Pet Cemetary.) I asked if the people know what happened and they said she "must have been beat up pretty bad" and added that it was a neighborhood cat. Awesome. So, I brought it in back where the other techs had set up oxygen and the crash kit and I opened the box. All I could see was the entire box and the cat moving as if I was seeing a TV station that wasn't coming in clearly. The cat wasn't moving, everything in the box was. Once my brain made sense of what I was seeing I realized there were ants everywhere. Next, I realized they were crawling out of the wound I had seen earlier. She turned out to have over 10 pucture wounds all over her face and neck that were necrotic and infested with ants and maggots. She also had a deep necrotic wound on her foot. We got word that the people who brought her in approved charges into the thousands of dollars, but the doctor convinced them that euthanisia was the most humane option.
5/19/2013: There were so many stability checks today that only 1 tech and 0 doctors got lunch. VCA provided pizza around 1pm. I finally got a slice around 5pm. A full day, but I prefer that to standing around doing nothing. I also got to participate in another large surgery today for more practice (an exploratory that also ended in euthanasia).
Saturday, May 4, 2013
Work Journal May 4, 2013
Friday: May 3, 2013
I was asked to help out in surgery today and the first surgery up was Joe Taylor's hind limb amputation. You might remember that he's the cat that had an open wound on it's tarsus and had a dislocated hip as well. Last week his surgery was delayed due to a nonregenerative anemia. This week his surgery was scheduled even though his anemia had not fully resolved. Oh, and he is also FIV+. For these reasons I was pretty nervous about monitoring him under anesthesia. It turned out that his surgery went very smoothly -his anesthesia was super smooth thanks to the doctors very skilled use at nerve blocks (both an epidural and a sciatic nerve block). The next surgery was just a healthy 3 year old Pomeranian's neuter. But, the poor thing just wouldn't stay under anesthesia. It was horrible and proved that you can't predict how an animal will react under anesthesia!
Saturday: May 4, 2013
"Stability Check on a dog who has been vomiting and not eating for four and a half days and now cannot walk". Turned out to be an 8 month old pitbull who was severely dehydrated, weak, and tachycardic. I asked the owner if he was vaccinated and she said yes, he came with all his shots when she got him. I asked how old he was when she got him and she said 9 weeks. She got all her puppy shots through us for her previous dog, so it is clear she was mislead by whoever sold her this pitbull puppy. It turned out to be Parvo positive. The dog was surrendered and we euthanized it.
"Stability Check on a kitten who's having trouble breathing". I ran out to the lobby and a giant man handed me a kitten the size of a mouse while pleading "you've got to save her, I'll do anything, pay anything". Seriously, maybe 7 days old. I didn't stop to ask any questions. The kitten was limp in my hands, cold but pink, the corneas slightly opague. On the way to the treatment area I didn't notice any breathing and I could not feel a heartbeat despite feeling his tiny ribs easily because he was so emaciated. We got him on oxygen right away and I started heating up a warmie while a fellow tech attempted to warm the kitten in his hands while the doctor checked for a heartbeat with a tiny pediatric stethoscope. There was a heartbeat, but it was slow. He was breathing, but slow. Another doctor ran to talk with the man about the situation to see how far he was willing to go to save the kitten. Like many cases we see due to our location, the man still insisted he wanted everything done, but admitted he had no money to pay us. After much back and forth while the kitten started going agonal. He finally agreed to surrender the kitten and we humanely euthanized the poor thing.
I was asked to help out in surgery today and the first surgery up was Joe Taylor's hind limb amputation. You might remember that he's the cat that had an open wound on it's tarsus and had a dislocated hip as well. Last week his surgery was delayed due to a nonregenerative anemia. This week his surgery was scheduled even though his anemia had not fully resolved. Oh, and he is also FIV+. For these reasons I was pretty nervous about monitoring him under anesthesia. It turned out that his surgery went very smoothly -his anesthesia was super smooth thanks to the doctors very skilled use at nerve blocks (both an epidural and a sciatic nerve block). The next surgery was just a healthy 3 year old Pomeranian's neuter. But, the poor thing just wouldn't stay under anesthesia. It was horrible and proved that you can't predict how an animal will react under anesthesia!
Saturday: May 4, 2013
"Stability Check on a dog who has been vomiting and not eating for four and a half days and now cannot walk". Turned out to be an 8 month old pitbull who was severely dehydrated, weak, and tachycardic. I asked the owner if he was vaccinated and she said yes, he came with all his shots when she got him. I asked how old he was when she got him and she said 9 weeks. She got all her puppy shots through us for her previous dog, so it is clear she was mislead by whoever sold her this pitbull puppy. It turned out to be Parvo positive. The dog was surrendered and we euthanized it.
"Stability Check on a kitten who's having trouble breathing". I ran out to the lobby and a giant man handed me a kitten the size of a mouse while pleading "you've got to save her, I'll do anything, pay anything". Seriously, maybe 7 days old. I didn't stop to ask any questions. The kitten was limp in my hands, cold but pink, the corneas slightly opague. On the way to the treatment area I didn't notice any breathing and I could not feel a heartbeat despite feeling his tiny ribs easily because he was so emaciated. We got him on oxygen right away and I started heating up a warmie while a fellow tech attempted to warm the kitten in his hands while the doctor checked for a heartbeat with a tiny pediatric stethoscope. There was a heartbeat, but it was slow. He was breathing, but slow. Another doctor ran to talk with the man about the situation to see how far he was willing to go to save the kitten. Like many cases we see due to our location, the man still insisted he wanted everything done, but admitted he had no money to pay us. After much back and forth while the kitten started going agonal. He finally agreed to surrender the kitten and we humanely euthanized the poor thing.
Saturday, April 27, 2013
Work Journal, April 27, 2013
Friday 4/19/2013:
Paraphimosis. Intact male Jack Russel -swelling reduced with powdered sugar and lube, then dextrose, mannitol, powdered sugar and lube. After the swelling went down some an eye hook was inserted between the prepuce and penis and used in a shoehorn fashion to get the penis in.
Maggoty Cancer Lump. 13yo? female Chow mix named Heidi -Was bit a week prior, owner brought her in due to his son's complaint that the dog smelled bad. Right side had ~8in circle of matted hair in the area of the bite. After shaving it a large lump was seen with two punctures on it. Shaving dislodged a large scab over one of the punctures which seeped tiny maggots. We squeezed the maggots out and flushed the wound. The dog went home on antibiotics and returned 2 days later for a recheck. No more maggots seen although the doctors are worried about the wounds' ability to heal on the lump. The lump was about 6cm in width and had some dark, necrotic looking skin on it. It had previously been aspirated as a sebaceous cyst, but a more current aspirate revealed only bloody serous fluid. The owner does not want the lump removed due to the dogs' age.
Saturday 4/20/2013:
A stability check was called on a dog bleeding from his eyes and mouth. We brought him back and it was true. He also had pinpoint petechiea on his mucous membranes (including his prepuce) and larger bruising on his lower abdomen. He was hyperemic as well. We got some blood and I made a smear to do a platelet count and got an optimistic 30,000 (it should be above 200,000). We transferred him to emergency (it was likely he'd need a blood transfusion) and their tests showed 12,000 platelets.
Sunday 4/21/2013:
We ran bloodwork on a previous hit by car cat (Joe Taylor) due for surgery the next day and found him to be extremely anemic (PCV of 12%). I took a blood smear and saw no signs of regeneration. Blood was sent to the lab and they confirmed no signs of regeneration. Surgery was cancelled and the cause of the anemia is being looked into.
Monday 4/22/2013:
A 3 year old pitbull came in on Sunday and was diagnosed with an open pyometra. Surgery was scheduled for today and had just completed as I started my shift. At her first TPR George found her mucous membranes to be nearly white and called the doctor. We put her on oxygen and checked her vitals including BP, but everything was WNL. We bolused LRS, gave 40cc's of Hetastarch, and then switched her fluids to 0.9% saline when her electrolytes were found to be off. After an hour or two she was more pink and more responsive and vocal, so she was put back in her cage and bupernorphine was given for pain management. An hour or two later, during a TPR her abdomen looked distended and the doctor was called for again. Another PCV was run and was 4% lower than the first one post surgery. Oxygen was started again, vitals still looked good, and she did pink up again although she remained lethargic. She ended up being transferred to emergency because we had no one on site to look after her overnight.
Wednesday 4/24/2013:
Otostrongylus season is upon the Marine Mammal Center. For the past couple weeks I've noticed animals bleeding from their injection sites long after the injections were given -a sign of the coagulopathy that signals the end stages of otostrongylus infection in elephant seal pups. "Oto" is a parasite of harbor seals that sometimes infects elephant seals. A successful parasite does not kill it's host, but oto often kills our ellies. There's no way to tell the statistics since there is no way to definitively diagnose oto except at necropsy where masses of worms are found in the pulmonary artery and clots are seen throughout the body systems. Today we had two critical oto suspect cases -an ellie named Brizo and another named Dance A Lot. Both were jaundice and lethargic in the morning, but in the afternoon Dance A Lot was scooped out of the pool nearly unresponsive. The vets gave fluids, dextrose (he had mildly low glucose levels), steroids, and antibiotics. A few hours later he was in the same situation. We ultrasounded him and found fluid in the chest which when tapped, was confirmed to be nearly straight blood which did not coagulate. DIC was the likely diagnosis and the animal was euthanized. Euthanasia is often seen by people outside the veterinary field to be an incredibly sad thing, but in cases like these where an animal is really suffering and the diagnosis is almost certain death it just feels like the right thing to do. I hope Dances A Lot is dancing over the rainbow bridge as we speak -see you on the other side, buddy!
Friday 4/27/13:
A 2 year old neutered male Yorkie came in as a stability check, the owners said they took his diaper off this afternoon and saw blood coming from his anus. We brought him back and found that serosanguineous fluid was dripping from his penis and there was a large (3-4 inch) area of swelling that felt a lot like a hernia just caudal to his prepuce. His vitals were all okay, but we called a doctor in to check the lump. They feared he had herniated his bladder and recommended that the owners bring him directly to an emergency clinic due to the fact that our ultrasound machine is broken and our surgeon was gone for the day.
Paraphimosis. Intact male Jack Russel -swelling reduced with powdered sugar and lube, then dextrose, mannitol, powdered sugar and lube. After the swelling went down some an eye hook was inserted between the prepuce and penis and used in a shoehorn fashion to get the penis in.
Maggoty Cancer Lump. 13yo? female Chow mix named Heidi -Was bit a week prior, owner brought her in due to his son's complaint that the dog smelled bad. Right side had ~8in circle of matted hair in the area of the bite. After shaving it a large lump was seen with two punctures on it. Shaving dislodged a large scab over one of the punctures which seeped tiny maggots. We squeezed the maggots out and flushed the wound. The dog went home on antibiotics and returned 2 days later for a recheck. No more maggots seen although the doctors are worried about the wounds' ability to heal on the lump. The lump was about 6cm in width and had some dark, necrotic looking skin on it. It had previously been aspirated as a sebaceous cyst, but a more current aspirate revealed only bloody serous fluid. The owner does not want the lump removed due to the dogs' age.
Saturday 4/20/2013:
A stability check was called on a dog bleeding from his eyes and mouth. We brought him back and it was true. He also had pinpoint petechiea on his mucous membranes (including his prepuce) and larger bruising on his lower abdomen. He was hyperemic as well. We got some blood and I made a smear to do a platelet count and got an optimistic 30,000 (it should be above 200,000). We transferred him to emergency (it was likely he'd need a blood transfusion) and their tests showed 12,000 platelets.
Sunday 4/21/2013:
We ran bloodwork on a previous hit by car cat (Joe Taylor) due for surgery the next day and found him to be extremely anemic (PCV of 12%). I took a blood smear and saw no signs of regeneration. Blood was sent to the lab and they confirmed no signs of regeneration. Surgery was cancelled and the cause of the anemia is being looked into.
Monday 4/22/2013:
A 3 year old pitbull came in on Sunday and was diagnosed with an open pyometra. Surgery was scheduled for today and had just completed as I started my shift. At her first TPR George found her mucous membranes to be nearly white and called the doctor. We put her on oxygen and checked her vitals including BP, but everything was WNL. We bolused LRS, gave 40cc's of Hetastarch, and then switched her fluids to 0.9% saline when her electrolytes were found to be off. After an hour or two she was more pink and more responsive and vocal, so she was put back in her cage and bupernorphine was given for pain management. An hour or two later, during a TPR her abdomen looked distended and the doctor was called for again. Another PCV was run and was 4% lower than the first one post surgery. Oxygen was started again, vitals still looked good, and she did pink up again although she remained lethargic. She ended up being transferred to emergency because we had no one on site to look after her overnight.
Wednesday 4/24/2013:
Otostrongylus season is upon the Marine Mammal Center. For the past couple weeks I've noticed animals bleeding from their injection sites long after the injections were given -a sign of the coagulopathy that signals the end stages of otostrongylus infection in elephant seal pups. "Oto" is a parasite of harbor seals that sometimes infects elephant seals. A successful parasite does not kill it's host, but oto often kills our ellies. There's no way to tell the statistics since there is no way to definitively diagnose oto except at necropsy where masses of worms are found in the pulmonary artery and clots are seen throughout the body systems. Today we had two critical oto suspect cases -an ellie named Brizo and another named Dance A Lot. Both were jaundice and lethargic in the morning, but in the afternoon Dance A Lot was scooped out of the pool nearly unresponsive. The vets gave fluids, dextrose (he had mildly low glucose levels), steroids, and antibiotics. A few hours later he was in the same situation. We ultrasounded him and found fluid in the chest which when tapped, was confirmed to be nearly straight blood which did not coagulate. DIC was the likely diagnosis and the animal was euthanized. Euthanasia is often seen by people outside the veterinary field to be an incredibly sad thing, but in cases like these where an animal is really suffering and the diagnosis is almost certain death it just feels like the right thing to do. I hope Dances A Lot is dancing over the rainbow bridge as we speak -see you on the other side, buddy!
Friday 4/27/13:
A 2 year old neutered male Yorkie came in as a stability check, the owners said they took his diaper off this afternoon and saw blood coming from his anus. We brought him back and found that serosanguineous fluid was dripping from his penis and there was a large (3-4 inch) area of swelling that felt a lot like a hernia just caudal to his prepuce. His vitals were all okay, but we called a doctor in to check the lump. They feared he had herniated his bladder and recommended that the owners bring him directly to an emergency clinic due to the fact that our ultrasound machine is broken and our surgeon was gone for the day.
Thursday, February 21, 2013
Elephant seal tears
Last week during my volunteer shift at Marine Mammal Center I was checking on all the animals before preparing for the first feed and I came upon a sleeping Northern Elephant Seal named Annabellini. I lingered awhile waiting for him to breathe so I knew he was okay, but I guess I disturbed him somehow. He stirred a little, moved a flipper and then opened his eyes. And that's when it happened: Two streams of water, one from each eye, shot out about 18 inches each -as if they came from a fat, hairy, double-barrelled squirt gun! A new volunteer was with me and said "Wow! What just happened?". In my (almost) year of experience I had never seen anything like that before, so I just said "Well, I guess he's well hydrated!".
After we finished feeding the animals on site I asked some fellow volunteers about what I had seen and in their (up to 20 years') experience none of them had ever seen an elephant seal shoot water from it's eyes. As we talked, Dr Lorraine passed by and she had no explanation either. At this point I started to feel a little silly and began doubting what I saw. But, Dr Francis Gulland came by later, so I explained what I saw one more time and asked if she had any idea what had happened. Of course she did. Seals lack nasolachrymal ducts! -I passively knew this, but not how it related to what I saw. Before I explain it any further, let me back up:
Anyone who has observed seals knows that when they are dry they often have a ring of wetness around their eyes. It is part of what makes them so cute -it often looks like they were crying. At Marine Mammal Center we recognize this as a sign of good hydration, but why do the tears spill out of the eyes in seals?
Most land mammals produce tears constantly, but the excess tears drain through a duct in the corner of the eye called the nasolacrymal duct which drains into the nose. This is why a person tends to get a runny nose when they cry! But, seals lack that duct so their tears just seep from their eyes constantly. (This is probably because they spend most of their time in the ocean where the draining of tears is not important.)
Here's a diagram of tear production in humans which is the same for most land mammals:
So, back to the dramatic event of an elephant seal shooting water from its eyes: Dr Gulland said that this was a sign that the seal was severely DEhydrated! She said that in his sleep, due to a decrease in tears, his eyelids likely sealed shut. The slow production of tears allowed the fluid to build up behind the eyelids. When I disturbed him and he opened his eyes the pressure was released causing the fluid to shoot out.
How cool is that?
Thursday, February 14, 2013
Comparing dog food prices
I just ran out of dog food and, once again, decided to re-evaluate the dog food I'm feeding since my budget is shrinking by quite a bit. I had been feeding Taste of the Wild, but wondered if another brand would be less expensive. Last week I went to check out prices for Purina Pro Plan or Purina One, but I was surprised to find out that on a price per pound basis they were about the same. Then I got to thinking this morning and remembered that when I had been feeding Purina One before I had to give much more per meal which meant I ran out faster. I wondered how to compare food pricing more accurately and came up with this (below). Yes it is math, no it's not hard, and I will I walk you through it and then provide a fool-proof worksheet in case you want to gather information and compare dog food prices yourself.
Let's say you have your choices narrowed down to 2:
Brand A's dog food is $35 for a 30lb bag.
Brand B's dog food is $45 for a 35lb bag.
You can determine price per pound by dividing the price by the number of pounds like this:
Brand A's cost per pound is: $35/30lbs = $1.17/lb
Brand B's cost per pound is: $45/35lbs = $1.29/lb
(And if you are like me and forget which number to divide by the other, just remember "price per pound" because that's the order you punch them in PRICE <divided by> # OF POUNDS. Easy!)
So, it seems at first glance that Brand A is the better deal. But, like I said before there is another tricky factor that most consumers don't think about and that is the recommended amount to feed your dog. Often high quality dog foods require you to feed your dog fewer cups of food because the ingredients are absorbed better (which also leads to less to clean up after the meal, if you know what I mean).
Unfortunately, dog food manufacturer's don't have to list the weight of their food by cup or the number of cups in the bag, so there is no precise way to calculate the number of feedings you'll get from a bag. But, I weighed a cup of Beneful weight management and it was 3oz. A cup of Chicken Soup Large Breed Adult food was 4oz per cup. So, I'm going to use 3.5oz per cup which means that 1lb = 4.6 cups. (And if you wonder how I got that: 16 ounces per pound divided by 3.5oz per cup = 3.5oz per cup.)
Brand A recommends 4 cups a day for your dog's body weight.
Brand B recommends 3 cups a day for your dog's body weight.
So, the cost of Brand A per day is:
4c per day / 4.6c per pound = 0.89lbs per day
0.89lbs * $1.17/lb = $1.04 per day to feed your dog this food.
And the cost of Brand B per day is:
3c per day / 4.6c per pound = 0.65lbs per day
0.65lbs * $1.29/lb = $0.84 per day to feed your dog this food.
So, despite our initial impression, Brand B is actually cheaper to feed than Brand A because, while the price is higher per pound, you don't have to feed as much of it.
Here's a worksheet to do this calculation yourself:
_______ price of food
DIVIDED BY:
_______ pounds per bag
EQUALS:
_______ price per pound
NEXT:
_______ number of cups per day to feed
DIVIDED BY:
4.6 cups per pound
OR weigh the food and divide 16oz by the number of ounces in a cup of the food to get actual cups per pound
EQUALS:
_______ number of pounds per day
NEXT:
_______ number of pounds per day (from above)
MULTIPLIED BY:
_______ price per pound (from above)
EQUALS:
_______ cost per day to feed that food
Let's say you have your choices narrowed down to 2:
Brand A's dog food is $35 for a 30lb bag.
Brand B's dog food is $45 for a 35lb bag.
You can determine price per pound by dividing the price by the number of pounds like this:
Brand A's cost per pound is: $35/30lbs = $1.17/lb
Brand B's cost per pound is: $45/35lbs = $1.29/lb
(And if you are like me and forget which number to divide by the other, just remember "price per pound" because that's the order you punch them in PRICE <divided by> # OF POUNDS. Easy!)
So, it seems at first glance that Brand A is the better deal. But, like I said before there is another tricky factor that most consumers don't think about and that is the recommended amount to feed your dog. Often high quality dog foods require you to feed your dog fewer cups of food because the ingredients are absorbed better (which also leads to less to clean up after the meal, if you know what I mean).
Unfortunately, dog food manufacturer's don't have to list the weight of their food by cup or the number of cups in the bag, so there is no precise way to calculate the number of feedings you'll get from a bag. But, I weighed a cup of Beneful weight management and it was 3oz. A cup of Chicken Soup Large Breed Adult food was 4oz per cup. So, I'm going to use 3.5oz per cup which means that 1lb = 4.6 cups. (And if you wonder how I got that: 16 ounces per pound divided by 3.5oz per cup = 3.5oz per cup.)
Brand A recommends 4 cups a day for your dog's body weight.
Brand B recommends 3 cups a day for your dog's body weight.
So, the cost of Brand A per day is:
4c per day / 4.6c per pound = 0.89lbs per day
0.89lbs * $1.17/lb = $1.04 per day to feed your dog this food.
And the cost of Brand B per day is:
3c per day / 4.6c per pound = 0.65lbs per day
0.65lbs * $1.29/lb = $0.84 per day to feed your dog this food.
So, despite our initial impression, Brand B is actually cheaper to feed than Brand A because, while the price is higher per pound, you don't have to feed as much of it.
Here's a worksheet to do this calculation yourself:
_______ price of food
DIVIDED BY:
_______ pounds per bag
EQUALS:
_______ price per pound
NEXT:
_______ number of cups per day to feed
DIVIDED BY:
4.6 cups per pound
OR weigh the food and divide 16oz by the number of ounces in a cup of the food to get actual cups per pound
EQUALS:
_______ number of pounds per day
NEXT:
_______ number of pounds per day (from above)
MULTIPLIED BY:
_______ price per pound (from above)
EQUALS:
_______ cost per day to feed that food
Wednesday, January 30, 2013
Elephant seal skin disease
We had a yearling Northern Elephant Seal come in to the Marine Mammal Center today. She is underweight and is reported to have blood in her urine. The most obvious issue, however, is that she has lesions all over her back and they are seeping blood tinged, grayish fluid. And she smells. Really bad.
Although she has not yet had an admit exam, I'm going to guess that she has Northern Elephant Seal Skin Disease (NESSD). I did a search on this condition and found a scientific paper from 1997:
http://www.ncbi.nlm.nih.gov/pubmed/9249688
It turns out that NESSD affects Northern Elephant Seals that are 9 months to 2 years old and most cases are seen between January and May. Moderate cases peak between December and January, severe cases are usually seen between March and May.
Northern Elephant Seal Skin Disease is graded as mild, moderate, or severe. Mild cases have ulcers that are less than 2cm in diameter or covering less than half of the body surface. Moderate cases have larger lesions with thickened skin, and severe cases have large ulcers that grow into one another, exude blood or fluid, and may become necrotic meaning that the tissue begins to die.
Based on the above grading scale, to me, the new elephant seal seems to have a moderate to severe case of NESSD. Mild cases have a survival rate of 93%, 66% survive moderate cases, and less than 1% survive severe cases. So, the chances for our new ellie aren't awesome if moderate to severe NESSD is her diagnosis. The cause of death in cases of NESSD is most often septicemia (going "septic" or an infection that takes over the entire body). This likely happens when bacteria enter through the skin lesions.
The next question might be what caused her condition? The study I read found no clear cause. Viruses were not found, bacterial cultures were taken but nothing but normal skin bacteria was found consistently. One interesting finding, however, is that affected seals tended to be smaller than unaffected ones. This may point to a genetic cause which could be explained by the population bottleneck that occurred in the early 1900's when the animals were down to around 100 individuals from which all present day Northern Elephant Seals arose.
It was also found that the skin lesions and blood work changes that happen in elephant seals affected with NESSD are also consistent with exposure to polyhalogenated aromatic hydrocarbons (PHAHs) including PCB's and PBB's.
According to wikipedia PCBs were used as coolants and insulating fluids for transformers and capacitors, such as those used in old fluorescent light ballasts, plasticizers in paints and cements, stabilizing additives in flexible PVC coatings of electrical wiring and electronic components, pesticide extenders, cutting oils, reactive flame retardants, lubricating oils, hydraulic fluids, and sealants, adhesives, wood floor finishes, paints, de-dusting agents, water-proofing compounds, casting agents, vacuum pump fluids, fixatives in microscopy, surgical implants, and in carbonless copy paper. They were banned in the US in the 1970's for most uses, but their use in closed applications such as capacitors has continued in the US and high concentrations have been found in recently in both water and on land.
PBBs are used as flame retardants, added to plastics used in products such as home electrical appliances, textiles, plastic foams, laptop cabinets, etc. to make them difficult to burn. Their use is restricted in the EU, but wikipedia says nothing about any US regulations.
Both the wikipedia articles on PCB's and PBB's list acne and skin issues among signs of exposure and apparently more research is being done on a possible link between these chemicals and Northern Elephant Seal Skin Disease.
Although she has not yet had an admit exam, I'm going to guess that she has Northern Elephant Seal Skin Disease (NESSD). I did a search on this condition and found a scientific paper from 1997:
http://www.ncbi.nlm.nih.gov/pubmed/9249688
It turns out that NESSD affects Northern Elephant Seals that are 9 months to 2 years old and most cases are seen between January and May. Moderate cases peak between December and January, severe cases are usually seen between March and May.
Northern Elephant Seal Skin Disease is graded as mild, moderate, or severe. Mild cases have ulcers that are less than 2cm in diameter or covering less than half of the body surface. Moderate cases have larger lesions with thickened skin, and severe cases have large ulcers that grow into one another, exude blood or fluid, and may become necrotic meaning that the tissue begins to die.
Based on the above grading scale, to me, the new elephant seal seems to have a moderate to severe case of NESSD. Mild cases have a survival rate of 93%, 66% survive moderate cases, and less than 1% survive severe cases. So, the chances for our new ellie aren't awesome if moderate to severe NESSD is her diagnosis. The cause of death in cases of NESSD is most often septicemia (going "septic" or an infection that takes over the entire body). This likely happens when bacteria enter through the skin lesions.
The next question might be what caused her condition? The study I read found no clear cause. Viruses were not found, bacterial cultures were taken but nothing but normal skin bacteria was found consistently. One interesting finding, however, is that affected seals tended to be smaller than unaffected ones. This may point to a genetic cause which could be explained by the population bottleneck that occurred in the early 1900's when the animals were down to around 100 individuals from which all present day Northern Elephant Seals arose.
It was also found that the skin lesions and blood work changes that happen in elephant seals affected with NESSD are also consistent with exposure to polyhalogenated aromatic hydrocarbons (PHAHs) including PCB's and PBB's.
According to wikipedia PCBs were used as coolants and insulating fluids for transformers and capacitors, such as those used in old fluorescent light ballasts, plasticizers in paints and cements, stabilizing additives in flexible PVC coatings of electrical wiring and electronic components, pesticide extenders, cutting oils, reactive flame retardants, lubricating oils, hydraulic fluids, and sealants, adhesives, wood floor finishes, paints, de-dusting agents, water-proofing compounds, casting agents, vacuum pump fluids, fixatives in microscopy, surgical implants, and in carbonless copy paper. They were banned in the US in the 1970's for most uses, but their use in closed applications such as capacitors has continued in the US and high concentrations have been found in recently in both water and on land.
PBBs are used as flame retardants, added to plastics used in products such as home electrical appliances, textiles, plastic foams, laptop cabinets, etc. to make them difficult to burn. Their use is restricted in the EU, but wikipedia says nothing about any US regulations.
Both the wikipedia articles on PCB's and PBB's list acne and skin issues among signs of exposure and apparently more research is being done on a possible link between these chemicals and Northern Elephant Seal Skin Disease.
Tuesday, January 29, 2013
Dr Internet
As a bright-eyed new tech who loves helping not only animals but the people who care for them I found /pets and /puppy101 on reddit.com and thought I'd share my knowledge. I answered a question on a cat who's not using his litterbox and a guy having issues with his aquarium and I felt all warm and fuzzy inside. Then I stumbled on "Help! I found this on my dog!". I clicked on it and it wasn't a photo of a tick or a flea. It was a blurry photo of a reddened area of skin with some hair missing. And the person added at the end that they can't take their dog to the vet because it costs too much.
I know this makes a lot of us in the veterinary medicine world really angry, but I want to look beyond that anger to see if there are ways that we can stem the tide of people seeking Dr Internet over their veterinarian.
I suppose the impression that this person got with his last vet visit was something like: My dog was fine, I was just a little concerned about this red bald patch so I took him to the vet and came away with one dose of medication and it cost me $250! Then they want me to come back for a recheck. I wonder how much it'll cost for them to tell me he's fine?
And from the clinic's point of view: The dog came in overdue for his vaccines, with a lapse in heartworm medication, sarcoptic mange was found to be the cause of the skin issue, but only after a skin scrape test. A dose of ivermectin was given and the dog was sent home vaccinated, with heartworm preventative, and a great prognosis!
So, on one side of the equation is very little value from the perspective of the client, and lots of value seen from the perspective of the hospital. I believe that bridging that gap is key. Apparently people out there believe that a diagnosis can be made with a photo or a description of symptoms. And I wonder -are they not being told about the range of possible causes and tests that are being done at their vet clinic in order to make the diagnosis?
Maybe we as vet staff need to place more of an emphasis on "we know how to get to the answer" rather than "we have the answer". The answer to most day-to-day questions can be googled and I think clients believe the answer to their medical questions is just as easily found on google. If that guess is correct, then I think it needs to be our job to educate people about how much work goes into making the diagnosis. That's what justifies the bill even if the answer is all they came looking for.
I know this makes a lot of us in the veterinary medicine world really angry, but I want to look beyond that anger to see if there are ways that we can stem the tide of people seeking Dr Internet over their veterinarian.
I suppose the impression that this person got with his last vet visit was something like: My dog was fine, I was just a little concerned about this red bald patch so I took him to the vet and came away with one dose of medication and it cost me $250! Then they want me to come back for a recheck. I wonder how much it'll cost for them to tell me he's fine?
And from the clinic's point of view: The dog came in overdue for his vaccines, with a lapse in heartworm medication, sarcoptic mange was found to be the cause of the skin issue, but only after a skin scrape test. A dose of ivermectin was given and the dog was sent home vaccinated, with heartworm preventative, and a great prognosis!
So, on one side of the equation is very little value from the perspective of the client, and lots of value seen from the perspective of the hospital. I believe that bridging that gap is key. Apparently people out there believe that a diagnosis can be made with a photo or a description of symptoms. And I wonder -are they not being told about the range of possible causes and tests that are being done at their vet clinic in order to make the diagnosis?
Maybe we as vet staff need to place more of an emphasis on "we know how to get to the answer" rather than "we have the answer". The answer to most day-to-day questions can be googled and I think clients believe the answer to their medical questions is just as easily found on google. If that guess is correct, then I think it needs to be our job to educate people about how much work goes into making the diagnosis. That's what justifies the bill even if the answer is all they came looking for.
Thursday, January 24, 2013
Alternative to No-Sorb
When you can't collect a urine sample from a cat and have to send home a kit with the owners a cheap alternative to No-Sorb is some aquarium gravel. We put it in washed baby food jars (we use baby food to distract animals while giving them vaccines or doing other procedures) and package it with a 3cc syringe (no needle) and a red top tube for them to put it in.
Oh, and remember to remind clients to wash their litterbox thoroughly before trying to collect a sample!
Oh, and remember to remind clients to wash their litterbox thoroughly before trying to collect a sample!
Thursday, January 3, 2013
Identifying demodex vs sarcoptes mange mites
To do a skin scraping you need:
Demodex mites are most commonly found because a small number live on pets normally, but an abnormal immune response can cause these mites' numbers to increase enough to cause clinical signs and require treatment. Usually these clinical signs are hair loss with or without itching that can lead to pyoderma and other secondary skin infections. It can occur locally, usually on the face or forelimbs and paws, or be generalized.
Some say demodex mites look like cigars. They are elongated and have eight legs that you may see moving on the front half of their body.
If demodex (demodectic mange) is diagnosed it should be noted that it is NOT contagious to humans or other pets in the household.
Sarcoptes mites are round, on the other hand, so they are easy to distinguish from demodex:
If sarcoptic mange is diagnosed it should be noted that it IS contagious to other pets who come in contact with the infected pet as well as humans. So, wash your hands thoroughly after handling animals with sarcoptic mange or, better yet, wear gloves and protective clothing if it is suspected.
Clinical signs of sarcoptic mange is intense pruritis (itchiness) and hair loss that begins on the ventral abdomen, chest, ears, elbows, and legs and, if left untreated, can become generalized.
- a dulled scalpel blade or other instrument for scraping
- a slide
- mineral oil
- a microscope
- Put a drop of mineral oil on the slide and dip the blade or scraper in the oil to lightly coat it so that the debris will stick to the blade.
- Choose an area of alopecia and scrape the skin with the blade until you begin to see blood. This is necessary because demodex mites live in hair follicles which are fairly deep under the surface of the skin. (Some say to pinch the skin while scraping it, but I've never seen this done in practice.)
- Clean debris off of the blade by dipping it in the mineral oil and wiping it off on the slide -do the best you can.
- Repeat the procedure using 3-5 different sites. This is important because sarcoptes (scabies) mites are hard to find.
Demodex mites are most commonly found because a small number live on pets normally, but an abnormal immune response can cause these mites' numbers to increase enough to cause clinical signs and require treatment. Usually these clinical signs are hair loss with or without itching that can lead to pyoderma and other secondary skin infections. It can occur locally, usually on the face or forelimbs and paws, or be generalized.
Some say demodex mites look like cigars. They are elongated and have eight legs that you may see moving on the front half of their body.
If demodex (demodectic mange) is diagnosed it should be noted that it is NOT contagious to humans or other pets in the household.
Sarcoptes mites are round, on the other hand, so they are easy to distinguish from demodex:
If sarcoptic mange is diagnosed it should be noted that it IS contagious to other pets who come in contact with the infected pet as well as humans. So, wash your hands thoroughly after handling animals with sarcoptic mange or, better yet, wear gloves and protective clothing if it is suspected.
Clinical signs of sarcoptic mange is intense pruritis (itchiness) and hair loss that begins on the ventral abdomen, chest, ears, elbows, and legs and, if left untreated, can become generalized.
Subscribe to:
Posts (Atom)